Stagescancer.net – Liver cancer is a serious condition that affects thousands of people every year. If you or a loved one has been diagnosed with liver cancer, you may have many questions, including what the life expectancy is for someone with this disease. The answer is complex and can depend on several factors, including the type and stage of liver cancer, age, overall health, and treatment options. Understanding survival rates and prognosis statistics can help individuals make informed decisions about their care and improve their overall quality of life. In this article, we will explore the different factors that can impact life expectancy in individuals with liver cancer and provide a comprehensive understanding of what to expect.
Throughout the article, we will delve into the various types and stages of liver cancer, examine the factors that can influence life expectancy, such as tumor characteristics, treatment options, and early detection, and highlight the importance of emotional support during this challenging time. We will also discuss palliative care and hospice services, clinical trials and experimental treatments, and survivorship care plans. By the end of this article, you will have a better understanding of the prognosis and life expectancy for individuals with liver cancer and the resources available to those affected by the disease.
Let’s begin by exploring the life expectancy of individuals diagnosed with liver cancer and the survival rates associated with the disease.
Types and Stages of Liver Cancer
Liver cancer can be categorized into several types, including hepatocellular carcinoma (HCC), cholangiocarcinoma, angiosarcoma, and hemangiosarcoma, among others. HCC is the most common type of liver cancer, accounting for about 75% of all cases. Cholangiocarcinoma, also known as bile duct cancer, occurs in the tubes that connect the liver and gallbladder to the small intestine. Other types are much rarer and can have distinct characteristics and treatments.
Stages of liver cancer refer to the extent and severity of the cancer and range from stage 1 (early-stage, localized cancer) to stage 4 (advanced cancer that has spread to other parts of the body). The stage of cancer is a crucial factor in determining prognosis and treatment options. Along with staging, tumor characteristics such as the size, number, and location of tumors also play a significant role in predicting outcomes.
Treatment Options by Stage
The stage of liver cancer can significantly impact the treatment options available for patients. For early-stage liver cancer, surgical resection is the preferred treatment option, with up to 70% of patients being eligible for surgery. Other treatments such as ablation therapy, embolization, and liver transplantation may also be utilized. For advanced cancer, palliative care can be used to relieve symptoms and improve quality of life. Chemotherapy, radiation therapy, and targeted therapies may also be employed, depending on the individual’s stage and tumor characteristics.
Factors Affecting Life Expectancy
When it comes to liver cancer, life expectancy can vary depending on several factors. Age, overall health, tumor size, and location, and the presence of metastasis can all impact a patient’s prognosis. Individuals need to speak with their healthcare providers to better understand how these factors may affect them.
Treatment options also play a critical role in determining life expectancy. For example, liver transplants and surgery may provide better outcomes for some patients. In contrast, individuals with advanced liver cancer may opt for palliative care to manage symptoms and improve their quality of life.
Doctors may use various tools and tests to assess an individual’s prognosis, such as tumor markers and imaging studies. These measures can help healthcare providers create a personalized treatment plan that is tailored to the individual’s needs and goals.
Age
Age can be a major factor in the prognosis and survival rates of liver cancer patients. Generally, individuals over the age of 60 are at a higher risk of developing liver cancer and may have lower survival rates compared to younger patients. This is likely due to age-related changes in the body, making it more difficult to tolerate treatment and recover from surgery.
Overall Health
Overall health is another crucial factor in determining life expectancy for liver cancer patients. Individuals with pre-existing conditions, such as diabetes or heart disease, may be at a higher risk of complications during treatment and have a poorer prognosis. Maintaining a healthy lifestyle through diet and exercise can help improve overall health and may improve outcomes for individuals with liver cancer.
| Factor | Impact on Life Expectancy |
|---|---|
| Tumor size and location | Larger tumors and tumors that are located in certain areas of the liver may be more difficult to remove and can impact survival rates. |
| Presence of metastasis | If the cancer has spread beyond the liver to other organs or areas of the body, it can be more challenging to treat and may shorten life expectancy. |
| Treatment options | Different treatments can have varying impacts on life expectancy. For example, liver transplantation may provide better outcomes for some individuals compared to chemotherapy. |
Individuals with liver cancer need to work closely with their healthcare providers to better understand their prognosis and identify the most appropriate treatment options. By taking an active role in their care, individuals can make informed decisions that positively impact their overall health and well-being.
Tumor Characteristics and Life Expectancy
The prognosis for liver cancer patients is heavily influenced by the characteristics of their tumors. Medical professionals consider many factors, including the number of tumors present, their size, and whether they have spread beyond the liver.
According to recent studies, liver cancer patients with a single tumor smaller than five centimeters have a five-year survival rate of approximately 50%, while those with multiple tumors or tumors larger than 5 cm have a much lower survival rate of around 20%. This survival rate decreases even further for individuals whose cancer has spread beyond the liver.
| Tumor Characteristics | Survival Rate |
|---|---|
| Single tumor smaller than 5 cm | 50% |
| Multiple tumors or tumors larger than 5 cm | 20% |
| The cancer spread beyond the liver | Less than 5% |
Treatment options, such as surgery or chemotherapy, may also depend on the characteristics of the tumor. Therefore, early detection and accurate diagnosis of tumor characteristics play a vital role in determining the best course of treatment and the outlook for patients.
Treatment Options and Impact on Prognosis
The treatment options for liver cancer vary depending on the stage of the cancer, the health of the patient, and the tumor characteristics. The goal of treatment is to remove the cancerous tissue or slow down the growth of the tumor while preserving normal liver function. Let’s examine how different treatments can affect life expectancy and consider the potential benefits and limitations of each approach.
Surgery and Liver Transplantation
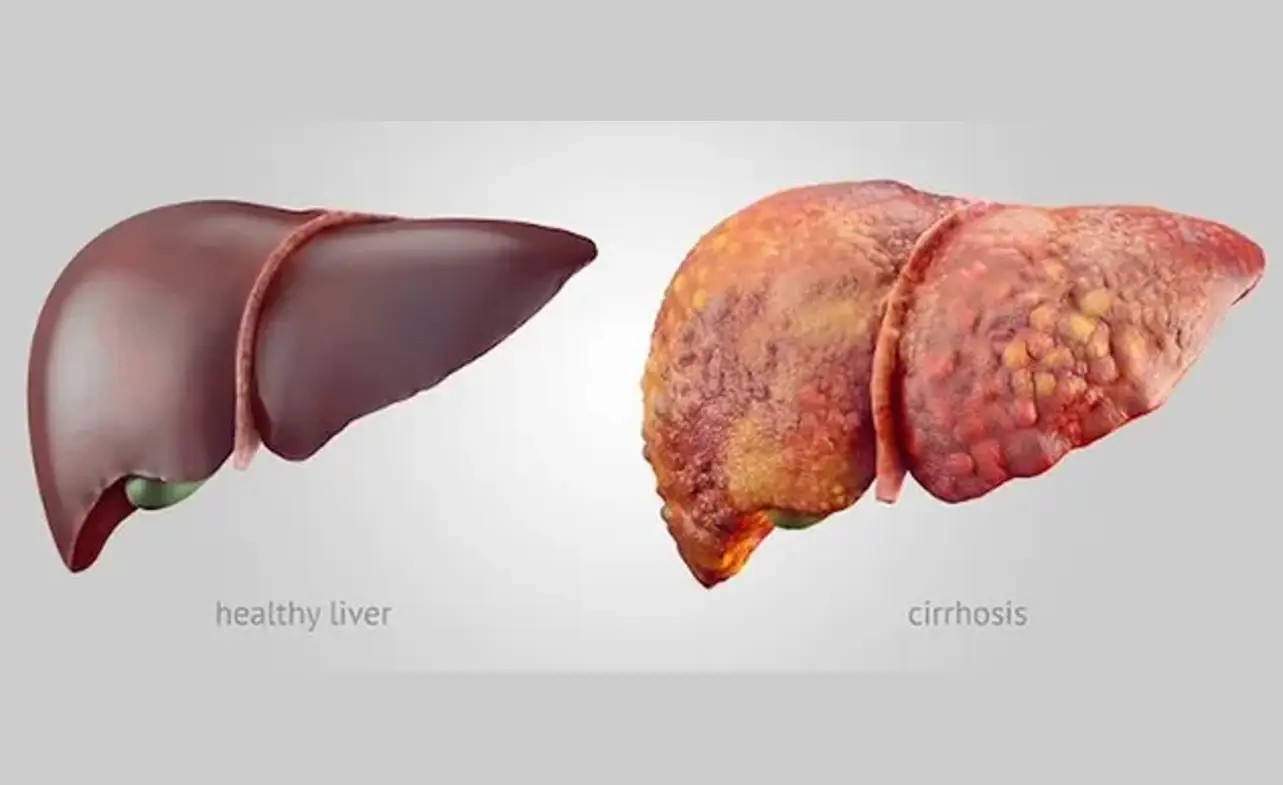
Surgery and liver transplantation are primary treatments for liver cancer patients. Surgical removal of the tumor or tumors is the most common way to treat liver cancer. If the tumor is small and localized, surgery can remove part of the liver and leave the remaining liver tissue to take over the liver functions. For advanced liver cancer, liver transplantation may be an option. This involves removing the diseased liver and replacing it with a healthy liver from a donor. The success of surgery and liver transplantation depends on the size and location of the tumor, the health of the patient, and the presence of cirrhosis or other liver diseases.
Radiation and Chemotherapy
Radiation therapy uses high-energy radiation to kill cancer cells. It can be used to shrink the tumor before surgery or to relieve symptoms in advanced cancer cases. Chemotherapy uses drugs to destroy cancer cells or slow down their growth. These drugs can be given orally, through injection, or directly into the liver. Both radiation therapy and chemotherapy have potential side effects, including nausea, vomiting, fatigue, and hair loss. They can also damage the liver and other healthy cells. The effectiveness of these treatments depends on the stage of the cancer, the patient’s overall health, and the location and size of the tumor.
Targeted Therapy
Targeted therapy is a newer approach to treating liver cancer that uses drugs to target specific molecules or proteins that are involved in the growth and spread of cancer cells. These drugs can be administered orally or through injection. Targeted therapy can cause fewer side effects than radiation or chemotherapy and can be effective in prolonging life in some patients. However, it is not effective for everyone and can be expensive.
Clinical Trials
Clinical trials are research studies that test new drugs or treatment approaches for liver cancer. They provide access to innovative therapies that may not be available through conventional treatment options. Patients participating in clinical trials can play a crucial role in discovering better treatments for liver cancer and improving survival rates. However, clinical trials have eligibility criteria, and not all patients are suitable candidates.
| Treatment Option | Potential Benefits | Limitations |
|---|---|---|
| Surgery and Liver Transplantation | Can provide a cure; preserves liver function; and can be used for both early and advanced stages of liver cancer. | Risks of complications and infection; limited availability; not suitable for all patients; can be expensive. |
| Radiation and Chemotherapy | Can shrink tumors before surgery; relieve symptoms; and may improve survival rates in some patients. | Potential side effects include damage to healthy cells, liver damage, and lowered immunity; effectiveness varies among patients; not curative. |
| Targeted Therapy | Can target specific molecules or proteins; with fewer side effects than radiation or chemotherapy. | Expensive; not effective for all patients; limited availability. |
| Clinical Trials | Access to innovative therapies not available through conventional options; potential for improved survival rates. | Eligibility criteria; potential risks and side effects; may not be effective for all patients. |
In conclusion, the choice of liver cancer treatment depends on several factors, including the stage and location of the tumor, the overall health of the patient, and the potential side effects and risks of each approach. Patients and their healthcare providers should weigh the benefits and limitations of each treatment option and make an informed decision that suits their individual needs. With early detection and appropriate treatment, liver cancer patients can improve their prognosis and achieve better overall outcomes.
The Importance of Early Detection
Early detection is crucial in the fight against liver cancer. Screening tests can help identify liver cancer at an early stage when treatment is most effective.
Regular screenings are recommended for individuals who are at a higher risk of developing liver cancer, such as those with a history of chronic liver disease, viral hepatitis, or heavy alcohol use. Other risk factors include obesity, diabetes, and exposure to certain chemicals and toxins.
Screening tests for liver cancer include blood tests, imaging tests such as ultrasounds, CT scans, MRIs, and biopsy. Talk to your doctor about which screening tests are appropriate for you and how often they should be performed.
It’s also important to take preventive measures to reduce the risk of developing liver cancer. These include maintaining a healthy diet and weight, limiting alcohol consumption, practicing safe sex, and getting vaccinated against hepatitis B and C.
Liver Cancer Survival Rates
When it comes to liver cancer prognosis, survival rates can provide valuable insights. Survival rates are typically based on five-year periods and are calculated based on various factors, including the stage of cancer and demographic data.
According to the American Cancer Society, the overall five-year survival rate for liver cancer is around 20%. However, survival rates vary significantly based on the stage of the disease and other factors.
| Stage of Liver Cancer | Relative Five-Year Survival Rate |
|---|---|
| Localized (confined to the liver) | Around 33% |
| Regional (spread to nearby lymph nodes or organs) | Around 11% |
| Distant (spread to distant organs or tissues) | Around 2% |
It is important to note that survival rates are statistical averages and do not necessarily predict the outcome for an individual diagnosed with liver cancer. Each case is unique, and many factors can influence life expectancy and prognosis.
Factors that may affect survival rates include age, overall health, tumor stage and size, and treatment options. Therefore, it is essential to seek medical advice and discuss with a healthcare provider the best course of action based on an individual’s specific diagnosis and situation.
Advances in Liver Cancer Treatment
Medical research has led to significant advances in liver cancer treatment in recent years, providing new hope and options for patients facing this challenging disease. Innovative therapies such as immunotherapy and targeted treatments have emerged, offering alternative approaches that can improve outcomes and support a better quality of life.
Immunotherapy is a type of treatment that harnesses the body’s immune system to recognize and attack cancer cells. This can be particularly effective in cases where traditional treatments have failed, offering renewed hope for many patients.
Targeted treatments, by contrast, work by targeting specific proteins or pathways that are involved in cancer cell growth. By doing so, these therapies can help slow or stop the spread of cancer cells and reduce the risk of the disease progressing.
| Treatment Type | Description | Potential Benefits |
|---|---|---|
| Immunotherapy | Uses the body’s immune system to fight cancer | Can be effective for patients who have not responded to conventional treatments |
| Targeted Therapy | Targets specific proteins or pathways involved in cancer cell growth | Can reduce the risk of disease progression and improve outcomes for some patients |
Despite these advances, much work remains to be done in the field of liver cancer treatment. Researchers continue to investigate new therapies and approaches to improve outcomes for patients, with ongoing clinical trials seeking to uncover promising new treatments.
If you or a loved one are facing a diagnosis of liver cancer, it’s important to seek out medical advice and explore all available treatment options. With the continued development of innovative therapies, new hope and possibilities are emerging for those fighting this challenging disease.
Side Effects and Quality of Life
Living with liver cancer can be challenging, especially when coping with its side effects. The side effects of liver cancer and its treatment can vary depending on the individual and the type and stage of cancer. Some of the common side effects experienced by liver cancer patients include:
- Fatigue: Feeling tired or weak most of the time
- Pain: In the abdomen, chest, or bones
- Nausea and vomiting: Feeling sick in the stomach and/or throwing up
- Loss of appetite and weight: Having little or no desire to eat and losing weight without trying
- Jaundice: Yellowing of the skin, eyes, and mucous membranes
- Mental health issues: Feeling anxious, depressed, or stressed
It’s important to inform your healthcare provider of any side effects you are experiencing, as they can recommend strategies to help manage and alleviate them. Strategies for managing side effects may include:
- Prescription medications to relieve pain, nausea, or anxiety
- Dietary changes to address weight loss or gastrointestinal issues
- Physical therapy to address weakness or pain
- Mental health interventions to address emotional stress
Along with managing side effects, maintaining a good quality of life is essential for liver cancer patients. Ways to improve overall well-being during treatment may include:
- Staying active, with low-impact exercises such as walking, yoga, or tai chi
- Eating a well-balanced diet, with plenty of fruits, vegetables, whole grains, and lean protein sources
- Engaging in stress-relieving activities such as meditation or deep breathing exercises
- Participating in support groups or counseling to connect with others who share similar experiences
Awareness of the potential side effects of liver cancer and its treatment, along with strategies for managing them, can help patients maintain a good quality of life during this challenging time.
Emotional Support and Coping Strategies
Receiving a liver cancer diagnosis can be overwhelming, and it’s normal to feel a range of emotions, including fear, anxiety, and sadness. Emotional support is an essential component of coping with the disease, and there are many resources available to help individuals and their loved ones through this challenging time.
Support Groups
Joining a support group can provide individuals with a sense of community and connection to others who are going through similar experiences. Many nonprofit organizations offer support groups either in-person or online, including the American Liver Foundation and Cancer Support Community.
Therapy and Counseling
Therapy and counseling can provide a safe space for individuals to express their emotions and work through difficult feelings. Mental health professionals can offer guidance and support to patients and their loved ones as they navigate treatment and recovery.
“It was a relief to connect with other people who understood what I was going through. I don’t feel so alone anymore.”
Self-Care Strategies
Practicing self-care can also help individuals cope with the emotional impact of liver cancer. This can include engaging in relaxing activities such as meditation or yoga, spending time with loved ones, and prioritizing rest.
Seeking Help
If you or a loved one is struggling with the emotional impact of liver cancer, it’s important to seek help. Talk to your healthcare team about resources and support networks that may be available to you.
Palliative Care and Hospice
For individuals with advanced liver cancer, palliative care and hospice services can provide comfort and support during end-of-life care. While often associated with death, palliative care can help patients live as fully and comfortably as possible, by addressing physical, emotional, and spiritual needs.
Palliative care can be provided alongside cancer treatments and is tailored to the individual’s needs. It may include pain management, symptom relief, counseling, and other therapies. Additionally, palliative care can provide support to family members and caregivers during this difficult time.
Hospice care is a type of palliative care designed for individuals in the final stages of life. Hospice care focuses on improving quality of life, rather than extending survival, and provides comfort and support to patients and their families. Hospice care services may include pain management, 24/7 nursing care, and emotional and spiritual support.
It is important to have discussions with healthcare providers and loved ones about end-of-life care options, including palliative care and hospice. By taking advantage of these services, patients and families can receive the emotional support and comfort they need during this challenging time.
Prognosis and Life Expectancy for Different Liver Cancer Types
Liver cancer encompasses a range of different types and subtypes, each with distinct characteristics and varying degrees of severity. The prognosis and life expectancy for individuals with liver cancer can vary greatly depending on the type of cancer they have been diagnosed with. Here, we outline the life expectancy and survival rates for some of the most common liver cancer types.
| Liver Cancer Type | Prognosis | Survival Rate |
|---|---|---|
| Hepatocellular carcinoma (HCC) | The most common type of liver cancer, HCC typically spreads through the liver and to other organs, resulting in a relatively poor prognosis. | For those with early-stage HCC, the 5-year survival rate can be as high as 70%. However, for those with advanced or metastatic HCC, the 5-year survival rate is typically less than 5%. |
| Cholangiocarcinoma | Cholangiocarcinoma is a rare type of liver cancer that forms in the bile ducts. It is notoriously difficult to detect in its early stages and, as a result, has a poorer prognosis compared to other liver cancers. | The 5-year survival rate for individuals with localized cholangiocarcinoma is around 30%, but this drops to less than 5% for those with metastatic cancer. |
| Angiosarcoma | This is a rare form of liver cancer that grows in the blood vessels of the liver. It can be difficult to treat, and its prognosis is generally poor. | The 5-year survival rate for individuals with this type of cancer is less than 10%. |
It’s important to remember that these statistics represent general trends and that each case of liver cancer is unique. Several factors can influence prognosis and life expectancy, including age, overall health, and the stage of the cancer at diagnosis. For the most accurate information about prognosis, individuals should consult with their healthcare team to discuss their specific case and treatment options.
Clinical Trials and Experimental Treatments
For individuals with liver cancer who have exhausted conventional treatment options, clinical trials and experimental treatments can offer new hope. Clinical trials are research studies that test new drugs, therapies, or procedures to determine their safety and effectiveness.
The Role of Clinical Trials
Clinical trials are a vital component of liver cancer research, providing opportunities for patients to access innovative therapies and contribute to the development of new treatments. By participating in a clinical trial, individuals can receive potentially life-saving treatments that are not yet available outside of a research setting. These trials also help researchers identify new ways to diagnose, treat, and prevent liver cancer.
Eligibility Criteria
Patient eligibility for a clinical trial varies depending on the specific study. Each trial has criteria for inclusion, such as age, health status, and stage of liver cancer. Patients must undergo a rigorous screening process to determine their eligibility and ensure their safety throughout the trial.
Potential Benefits
Participating in a clinical trial can offer potential benefits beyond conventional treatment methods. In addition to gaining access to new therapies, patients may receive more frequent monitoring and personalized care. They may also experience an improved quality of life and a sense of empowerment, knowing that they are contributing to progress in liver cancer research.
Experimental Treatments
Experimental treatments are therapies that are not yet approved by the U.S. Food and Drug Administration (FDA) but are available through clinical trials. These treatments may include immunotherapies, targeted therapies, and gene therapies, among others. While experimental treatments carry risks, they also offer potential benefits for patients with no other treatment options.
Resources for Finding Clinical Trials
There are several resources available to patients seeking clinical trials for liver cancer. The National Cancer Institute (NCI) maintains a comprehensive database of clinical trials, and many hospitals and cancer centers offer their clinical trials. Patients can also consult with their healthcare providers and liver cancer specialists for guidance on finding clinical trials that are appropriate for their needs.
Survivorship and Follow-up Care
Surviving liver cancer can be a relief, but it’s only the beginning of a new journey. Patients require ongoing follow-up care to address potential recurrence and monitor their overall health. In this section, we will discuss the different aspects of survivorship and follow-up care for liver cancer patients.
Survivorship Care Plans
Survivorship care plans are essential for liver cancer survivors. These plans outline the necessary tests and screenings to detect any recurring disease early on. Patients should work closely with their healthcare providers to develop these plans, which may include follow-up appointments, imaging tests, liver function tests, and blood tests.
Recommended Screenings
After liver cancer treatment, survivors require regular screenings to monitor their health. The recommended screening schedule may vary depending on the individual’s risk factors and overall health. However, patients should expect to undergo imaging tests, such as CT or MRI scans, at least every six months for the first two years, followed by annual testing. Liver function tests and blood tests may also be recommended regularly to track liver function.
The Importance of a Healthy Lifestyle
Maintaining a healthy lifestyle is paramount for liver cancer survivors. Adopting healthy habits, such as a balanced diet, regular exercise, and stress management, can help improve physical and mental well-being. Alcohol consumption should be avoided or limited to prevent further damage to the liver and reduce the risk of liver cancer recurrence.
Follow-up with Healthcare Providers
Survivors should stay in touch with their healthcare providers throughout the survivorship journey. Patients should use these appointments to discuss any changes in their health or well-being, ask questions, and voice concerns. It’s essential to have a good working relationship with your healthcare team to ensure that you receive the best-continuing care possible.
Liver Cancer Support Resources and Inspiring Patient Stories
Receiving a liver cancer diagnosis can be overwhelming, but you’re not alone. There are numerous support resources available to help you and your loved ones navigate this challenging time.
The American Cancer Society offers a wealth of information on liver cancer, including treatment options, coping strategies, and support services. They have a 24/7 helpline where you can speak with a trained professional for emotional support and practical advice.
The Liver Cancer Connect community is a great place to connect with others affected by liver cancer. This community offers a forum for sharing experiences and asking questions, as well as access to expert advice from liver cancer specialists.
The Cancer Support Community is another excellent resource for individuals with liver cancer. They offer online and in-person support groups, educational resources, and a helpline staffed by licensed professionals.
While liver cancer can be a challenging diagnosis, many inspiring patient stories offer hope and encouragement. From individuals who have successfully undergone treatment to those living with the disease, hearing from others who have walked a similar path can provide inspiration and motivation.
One such story is that of Anita Mitchell, who was diagnosed with liver cancer in 2015. Despite undergoing multiple surgeries and treatments, she remained optimistic throughout her journey. Today, Anita is cancer-free and serves as an advocate for liver cancer awareness and education.
Another inspiring story is that of Tom Nealon, who was diagnosed with liver cancer in 2003. After undergoing a liver transplant and radiation therapy, Tom became an avid supporter of cancer research and patient advocacy. Today, he continues to inspire others through his advocacy work and writing.
Remember, there is always hope and support available. Don’t hesitate to reach out for assistance and connect with others who understand what you’re going through. Together, we can fight liver cancer and improve outcomes for all.
FAQ
What is the life expectancy of someone with liver cancer?
The life expectancy of individuals diagnosed with liver cancer can vary depending on various factors. These factors include the stage of the cancer, the overall health of the individual, and the treatment options available. It is important to consult with a healthcare professional to get a personalized prognosis and understanding of what to expect.
What are the types and stages of liver cancer?
Liver cancer can be classified into different types, such as hepatocellular carcinoma (HCC) and cholangiocarcinoma. The stages of liver cancer are determined by the size and extent of the tumor and whether it has spread to other parts of the body. Understanding the type and stage of liver cancer is essential in determining the appropriate treatment and prognosis.
What factors can affect the life expectancy of someone with liver cancer?
The life expectancy of someone with liver cancer can be influenced by several factors, including age, overall health, tumor size, presence of metastasis (spread), and treatment options. These factors can vary from person to person, and it is important to discuss them with a healthcare professional to better understand their impact on prognosis.
How do tumor characteristics affect life expectancy in liver cancer?
Tumor characteristics, such as the number of tumors, their size, and whether they have spread beyond the liver, play a crucial role in determining life expectancy for patients with liver cancer. These characteristics can help in assessing the stage of the cancer and planning the most appropriate treatment approach.
How do treatment options impact life expectancy in liver cancer patients?
Treatment options for liver cancer can vary depending on the stage and characteristics of the tumor. Treatments such as surgery, liver transplantation, radiation therapy, chemotherapy, and targeted therapies can all have an impact on life expectancy. It is important to consult with a healthcare professional to understand the potential benefits and limitations of each treatment option.
Why is early detection important in liver cancer?
Early detection of liver cancer is crucial because it can significantly improve the chances of successful treatment. Regular screenings, especially for individuals with risk factors associated with liver cancer, can help detect the disease at an early stage when it is more treatable. Taking preventive measures and being aware of the symptoms can also aid in early detection.
What are the survival rates for liver cancer?
Survival rates for liver cancer can vary depending on different factors, such as the stage of the cancer and age group. It is important to note that survival rates are statistical averages and can’t predict an individual’s exact prognosis. Consulting with a healthcare professional is crucial to getting personalized information and a comprehensive understanding of survival rates.
What are the advances in liver cancer treatment?
Medical advancements in liver cancer treatment have led to innovative therapies such as immunotherapy and targeted therapies. These advancements have provided new options for patients and improved outcomes for some individuals. It is important to stay informed about the latest advances and consult with a healthcare professional to determine the most suitable treatment approach.
What are the common side effects of liver cancer and its treatment?
Liver cancer and its treatment can have significant side effects that can affect an individual’s quality of life. Common side effects may include fatigue, nausea, loss of appetite, and pain. It is important to work closely with a healthcare team to manage these side effects and improve overall well-being during treatment.
How can individuals cope with a liver cancer diagnosis?
Dealing with a diagnosis of liver cancer can be emotionally challenging. It is important to seek emotional support from loved ones, support groups, and healthcare professionals. Coping strategies such as maintaining a positive mindset, engaging in relaxation techniques, and accessing counseling services can also help individuals navigate through this difficult time.
What is the role of palliative care and hospice in liver cancer?
For individuals with advanced liver cancer, palliative care and hospice services can provide comfort and support. Palliative care focuses on managing symptoms and improving quality of life, while hospice care provides end-of-life support. It is crucial to have open discussions with healthcare professionals and loved ones to make informed decisions about palliative care and hospice services.
How does prognosis and life expectancy differ for different types of liver cancer?
Different types of liver cancer, such as hepatocellular carcinoma (HCC) and cholangiocarcinoma, have unique characteristics that can affect prognosis and life expectancy. It is important to consult with a healthcare professional to understand the specific prognosis associated with the type of liver cancer diagnosed.
What is the role of clinical trials and experimental treatments in liver cancer?
Clinical trials and experimental treatments can offer new options for individuals with liver cancer who have exhausted conventional treatment methods. These trials aim to evaluate the safety and effectiveness of new therapies. It is important to discuss eligibility criteria and potential benefits with healthcare professionals to determine if participation in a clinical trial is a suitable option.
What is the importance of survivorship care and follow-up for liver cancer?
After completing treatment for liver cancer, survivors require ongoing follow-up care to monitor their health and address any potential recurrence or long-term effects. Survivorship care plans, recommended screenings, and maintaining a healthy lifestyle are essential for maximizing long-term well-being. Regular communication with healthcare professionals is vital to ensure appropriate follow-up care.
What support resources are available for individuals with liver cancer?
There are numerous resources, organizations, and support groups available to provide assistance and emotional support to individuals with liver cancer and their caregivers. These resources can offer valuable information, guidance, and the opportunity to connect with others who are going through similar experiences. Patient stories can also be a source of inspiration and hope for individuals facing a liver cancer diagnosis.