Stagescancer.net – Pancreatic cancer is a severe illness that can often spread to other parts of the body, such as the liver. When pancreatic cancer spreads to the liver, known as liver metastasis, it becomes even more challenging to treat. Sadly, the survival rates for pancreatic cancer with liver metastasis are low, and the prognosis can be poor.
This article will explore the connection between pancreatic cancer and liver metastasis, the prognosis for this advanced stage of cancer, and the potential treatment options available. We will delve into various therapeutic approaches, including surgical interventions, chemotherapy, targeted therapy, and the latest immunotherapy advancements. We will also address the importance of palliative care, symptom management, emotional support, and psychosocial care for individuals living with this challenging condition.
Join us as we examine the latest research and future directions for managing pancreatic cancer that has spread to the liver. If you or a loved one has been diagnosed with pancreatic cancer spread to the liver, this article aims to provide you with the necessary information to make informed decisions about your disease and care options.
Understanding Pancreatic Cancer
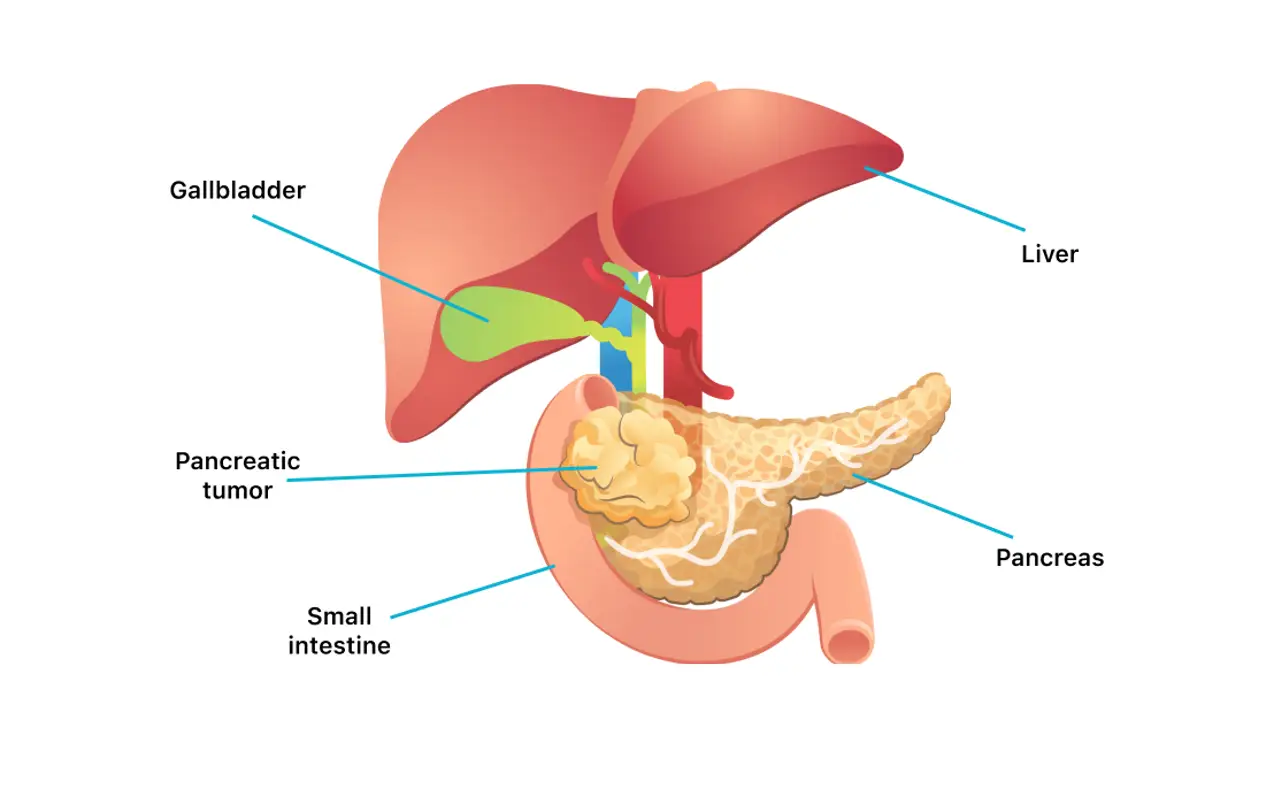
Pancreatic cancer occurs when abnormal cells in the pancreas grow and divide uncontrollably, forming a mass or tumor. While the exact cause of pancreatic cancer is not fully understood, certain risk factors increase the likelihood of developing this disease. These risk factors include:
- Age – most patients are over 65 years of age
- Smoking
- Obesity
- Family history
- Chronic inflammation of the pancreas (pancreatitis)
Common symptoms of pancreatic cancer may include:
- Jaundice (yellowing of the skin and eyes)
- Abdominal or back pain
- Unexplained weight loss
- Nausea and vomiting
- Fatigue or weakness
Diagnosis of pancreatic cancer may involve imaging tests, blood tests, and biopsies. Treatment options depend on the stage and extent of cancer and may include surgery, chemotherapy, radiation therapy, or a combination of these therapies.
Liver Metastasis in Pancreatic Cancer
Pancreatic cancer can be an aggressive disease that spreads to other organs, including the liver. When cancer cells move from the pancreas to the liver, it is referred to as liver metastasis.
Understanding the Spread of Pancreatic Cancer
Doctors use a staging system to determine the extent of pancreatic cancer spread. This helps doctors identify the best treatment options for patients with liver metastasis.
| Stage | Description |
|---|---|
| Stage 0 | Cancer cells are in the pancreas and have not spread elsewhere. |
| Stage I | Cancer cells have grown into nearby tissue, but have not spread to other organs. |
| Stage II | Cancer cells have spread to nearby lymph nodes, but not to other organs. |
| Stage III | Cancer cells have spread to nearby blood vessels. |
| Stage IV | Cancer cells have spread to distant organs, such as the liver. |
In most cases, liver metastasis from pancreatic cancer indicates stage IV disease. This is the most advanced stage, and treatment options may be limited.
Diagnosing Liver Metastasis from Pancreatic Cancer
To diagnose liver metastasis, doctors will use imaging tests such as CT scans, MRIs, or PET scans. These tests can show the spread of cancer cells to the liver.
If doctors suspect liver metastasis, they may order a liver biopsy. This involves using a needle to remove a small piece of liver tissue to test for cancer cells.
Treatment for Liver Metastasis from Pancreatic Cancer
There are several treatment options available to manage liver metastasis from pancreatic cancer, including:
- Surgery: Some patients may be eligible for surgery to remove cancerous tissue from the liver.
- Chemotherapy: Chemotherapy drugs can help slow the growth and spread of cancer cells in the liver and elsewhere.
- Targeted therapy: This treatment approach targets specific cancer cells to slow or stop the growth of cancer.
- Immunotherapy: This type of therapy harnesses the body’s immune system to fight cancer cells.
The treatment approach may depend on the extent of cancer spread, overall health, and individual patient needs.
Prognosis for Pancreatic Cancer with Liver Metastasis
Individuals with pancreatic cancer that has spread to the liver, known as liver metastasis, face a significant challenge as the prognosis for this advanced stage of cancer remains poor. According to the American Cancer Society, the five-year survival rate for pancreatic cancer that has spread to distant parts of the body, including the liver, is approximately 3%. However, some individuals may survive longer based on specific prognostic factors.
Prognostic Factors
Several factors can impact an individual’s survival with pancreatic cancer and liver metastasis. These factors include:
- The size and number of liver metastasis
- The stage of pancreatic cancer and how far it has spread
- The individual’s general health and overall response to treatment
- Genetic or molecular factors that may influence cancer growth and response to therapy
Prognosis Based on Specific Factors
Studies have found that individuals with a single liver metastasis that is smaller than 3 centimeters may have a better prognosis than those with multiple lesions or larger tumors. Similarly, if pancreatic cancer has not spread beyond the liver, surgical resection of the metastasis may be an option, which can improve survival rates.
The response to treatment also plays a significant role in an individual’s prognosis. While pancreatic cancer with liver metastasis is challenging to treat, combination chemotherapy regimens and targeted therapies have shown promise in slowing cancer growth and extending survival rates.
Overall Outlook
It is essential to note that each person’s journey with pancreatic cancer and liver metastasis is unique, and survival rates and prognostic factors can vary significantly. Healthcare providers can work with individuals to develop individualized treatment plans that aim to improve quality of life and extend survival rates.
Factors Affecting Survival Time
Survival time for individuals with pancreatic cancer and liver metastasis can vary greatly based on several factors. It’s essential to consider various elements when evaluating a prognosis, and healthcare providers typically do this by analyzing potential prognostic factors.
Prognostic Factors
Prognostic factors for pancreatic cancer with liver metastasis can include an individual’s overall health, age, and the extent of the cancer spread. Genetics can also influence survival time, as can the effectiveness of treatment.
Effectiveness of Treatment
Another critical factor that can influence survival time is the treatment response. If the individual responds positively to treatment, they may have a better prognosis compared to those who do not respond as well.
Treatment Options
Treatment options for pancreatic cancer with liver metastasis can include surgery, chemotherapy, targeted therapy, and immunotherapy. The most effective treatment depends on several factors, including the extent of cancer spread and an individual’s overall health.
| Treatment Option | Potential Survival Benefit |
|---|---|
| Surgery | May provide the most significant survival benefit for select individuals with localized liver metastasis |
| Chemotherapy | Can improve survival time in individuals with advanced pancreatic cancer that has spread to the liver |
| Targeted Therapy | May be helpful for individuals with specific genetic mutations |
| Immunotherapy | Can potentially boost the immune system to fight cancer cells and improve survival time |
It’s crucial to discuss all available treatment options with a healthcare provider to determine the best course of action.
Overall Health
Individuals with pancreatic cancer and liver metastasis who maintain good overall health generally have a better prognosis compared to those who have existing health conditions or comorbidities. This highlights the importance of maintaining a healthy lifestyle, including regular exercise and a balanced diet.
Moreover, maintaining emotional health through accessible psychosocial care can boost an individual’s overall well-being and quality of life and potentially positively influence survival time.
Treatment Options for Pancreatic Cancer Spread to the Liver
When pancreatic cancer spreads to the liver, treatment options depend on several factors, including the stage of cancer and the overall health of the individual. Here are some of the main treatment options:
| Treatment Type | Description |
|---|---|
| Surgery | In some cases, surgical removal of the affected areas of the liver may help extend the individual’s life. Liver transplant may also be considered in some cases, although it is typically only an option for those who have small tumors and meet certain criteria. |
| Chemotherapy | Chemotherapy drugs can be used to slow or halt the growth of cancer cells. Combination therapy, which involves using multiple chemotherapy drugs, may be more effective than using just one drug. Chemotherapy can cause side effects, such as hair loss, nausea, and fatigue, which can be managed with medication and other supportive measures. |
| Targeted Therapy | Targeted therapy drugs can block specific molecules that promote cancer growth. These drugs are often used in combination with chemotherapy or other treatments. Targeted therapy can cause side effects, such as skin rash, diarrhea, and high blood pressure. |
| Immunotherapy | Immunotherapy drugs can help the immune system recognize and attack cancer cells. Checkpoint inhibitors are a type of immunotherapy drug that block certain proteins that help cancer cells evade detection by the immune system. Immunotherapy can cause side effects, such as fatigue, skin rash, and diarrhea. |
Other treatment options for pancreatic cancer with liver metastasis may include radiation therapy, clinical trials, and palliative care. The best course of treatment will depend on the individual’s unique circumstances and should be determined in consultation with their healthcare team.
Surgical Approaches for Liver Metastasis
When pancreatic cancer spreads to the liver, surgical interventions may be recommended to manage the condition. Two primary surgical options are resection and ablation, both useful in particular cases but present varying levels of risk and effectiveness. It’s essential to have a thorough discussion with your healthcare provider to determine the most suitable course of treatment for you.
Resection
Surgical resection involves the removal of the metastatic liver tumor(s) via surgery. Depending on where the tumor(s) is located in the liver, different types of resection can be applied, such as hemihepatectomy for larger lesions and segmentectomy for smaller ones. Resection, however, is only successful in a limited number of cases due to the high risk of postoperative complications. Furthermore, this approach often requires a high level of surgical expertise to achieve complete removal of the tumor(s) and potentially prolong survival.
Ablation
Ablation, on the other hand, involves the destruction of cancerous cells or tissue. The procedure may be done using either surgical or nonsurgical approaches, including open surgery, laparoscopic surgery, and percutaneous techniques. Ablation is best suited to treat small to medium-sized tumors. Still, its effectiveness can decrease for larger tumors, particularly those located near the center of the liver. Potential risks may include bleeding, infection, and liver dysfunction.
| Resection | Ablation | |
|---|---|---|
| Effectiveness | Removes tumor(s) for potential cure. High success for small- to mid-sized tumors | Destroys tumor(s) but is often less effective than resection for larger tumors |
| Risk and complications | High risk of complications, requires a highly skilled surgeon | Less invasive with fewer complications, but potential risks may still occur |
| Recovery time | Lengthy recovery time, up to several months to regain normal function | Shorter recovery time, days to weeks for most patients |
Ultimately, the choice of surgical approach will depend on various factors, such as the location and size of the tumor(s) in the liver and the patient’s overall health. In some cases, doctors may recommend a combination of surgery and other treatment options, such as chemotherapy or radiation therapy, to improve the chances of successful treatment.
Consult with your medical team to determine the best course of action for managing pancreatic cancer with liver metastasis.
Chemotherapy for Pancreatic Cancer Spread to the Liver
Chemotherapy is a standard treatment option for individuals with pancreatic cancer that has spread to the liver. The goals of chemotherapy in this setting are to shrink the tumors, slow down their growth, and relieve symptoms such as pain and jaundice.
There are several chemotherapy drugs available to treat pancreatic cancer with liver metastasis, and the choice of drug(s) depends on various factors such as the individual’s overall health, the extent of cancer spread in the liver, and previous treatments received.
A combination of chemotherapy drugs may be used to achieve better results, and this is known as combination therapy. One common chemotherapy regimen for pancreatic cancer with liver metastasis uses a combination of drugs called FOLFIRINOX, which consists of four drugs: fluorouracil, leucovorin, irinotecan, and oxaliplatin.
While chemotherapy can be effective in managing pancreatic cancer with liver metastasis, it can also cause some side effects. Common side effects of chemotherapy include nausea, vomiting, hair loss, fatigue, and increased risk of infections.
It is essential to work closely with healthcare professionals to manage side effects and adjust treatment, ensuring that individuals can continue to receive the full benefits of chemotherapy.
| Chemotherapy Drugs | Common Side Effects |
|---|---|
| Fluorouracil (5-FU) | Nausea, vomiting, diarrhea, mouth sores |
| Gemcitabine (Gemzar) | Nausea, vomiting, hair loss, fatigue |
| FOLFIRINOX | Nausea, vomiting, diarrhea, hair loss, fatigue, increased risk of infections |
Chemotherapy has been shown to improve survival rates in individuals with advanced pancreatic cancer with liver metastasis. However, it is crucial to weigh the potential benefits and risks of chemotherapy with healthcare professionals and work collaboratively to decide on the best treatment approach for an individual’s specific situation.
Targeted Therapy for Pancreatic Cancer with Liver Metastasis
Targeted therapy is a type of cancer treatment that aims to block the growth and spread of cancer cells by identifying specific molecular targets on the surface of cancer cells. It is a promising treatment option for individuals with pancreatic cancer that has spread to the liver.
By targeting specific molecular targets on cancer cells, targeted therapy drugs can be more effective in destroying cancer cells than traditional chemotherapy drugs, which target all rapidly dividing cells, including healthy ones.
One example of a targeted therapy drug for pancreatic cancer with liver metastasis is erlotinib. This drug works by inhibiting the activity of a protein called epidermal growth factor receptor (EGFR) that is commonly overexpressed in pancreatic cancer cells. Other targeted therapy drugs that are being investigated in clinical trials include trastuzumab, which targets human epidermal growth factor receptor 2 (HER2), and bevacizumab, which targets vascular endothelial growth factor (VEGF).
Potential Effectiveness of Targeted Therapy
Targeted therapy has shown promising results in clinical trials for treating pancreatic cancer with liver metastasis. In a phase III clinical trial, erlotinib revealed a modest increase in survival rates when used in combination with chemotherapy compared to chemotherapy alone. Other studies have shown that targeted therapy drugs can help slow down cancer progression and improve overall survival rates.
Molecular Targets for Targeted Therapy
| Molecular Target | Targeted Therapy Drug |
|---|---|
| EGFR | Erlotinib |
| HER2 | Trastuzumab |
| VEGF | Bevacizumab |
Table: Examples of Molecular Targets and Targeted Therapy Drugs for Pancreatic Cancer with Liver Metastasis.
Targeted therapy offers a potentially effective solution for individuals with pancreatic cancer that has spread to the liver. As research continues to uncover new molecular targets, more effective targeted therapy drugs will likely become available to individuals with this condition.
Immunotherapy Advancements for Pancreatic Cancer with Liver Metastasis
Immunotherapy involves using the body’s immune system to fight cancer by identifying and attacking cancer cells.
Recent advancements in immunotherapy have shown promise in the treatment of pancreatic cancer that has spread to the liver. Clinical trials investigating the use of checkpoint inhibitors, a type of immunotherapy, have yielded encouraging results.
| Checkpoint Inhibitor | Drug Name | Targeted Molecule | Clinical Trial Results |
|---|---|---|---|
| PD-1 inhibitor | Pembrolizumab | PD-1 receptor | Promising response rates observed in pancreatic cancer with liver metastasis |
| CTLA-4 inhibitor | Ipilimumab | CTLA-4 receptor | Ongoing clinical trials investigating the potential efficacy in pancreatic cancer with liver metastasis |
Checkpoint inhibitors work by blocking proteins that inhibit the immune system’s ability to recognize and attack cancer cells. By doing so, they can help activate the immune system to fight the cancer. The PD-1 inhibitor pembrolizumab has shown promising results in pancreatic cancer with liver metastasis, with favorable response rates observed in clinical trials.
However, not all patients experience the same level of benefit from checkpoint inhibitors. Factors such as tumor mutational burden, cancer genetics, and immune system function can impact treatment response and overall outcomes.
As with other types of cancer treatments, there are potential side effects associated with checkpoint inhibitors, including skin rashes, fatigue, and gastrointestinal issues. Patients need to discuss the potential risks and benefits of immunotherapy with their healthcare providers.
Further research is needed to determine the optimal use of immunotherapy in the treatment of pancreatic cancer with liver metastasis. Several ongoing clinical trials are investigating the potential efficacy of combinations of checkpoint inhibitors with other treatments, such as chemotherapy and targeted therapy.
Palliative Care and Supportive Treatments
It is essential to focus on palliative care and supportive treatments to provide relief for individuals with pancreatic cancer and liver metastasis. Palliative care aims to improve the quality of life by managing symptoms such as pain, nausea, fatigue, and depression.
Supportive treatments can also be used to manage symptoms and side effects that may arise from other treatments such as chemotherapy or radiation therapy. Symptom management may include medication management or invasive procedures such as nerve blocks or stents.
Moreover, psychotherapy, counseling, and support groups can help address the psychosocial needs of individuals and their families who are dealing with this challenging diagnosis. This support can play a crucial role in managing depression, anxiety, and other mental health issues in patients and their families.
In conclusion, palliative care and supportive treatments play a vital role in managing symptoms, improving quality of life, and meeting the psychosocial needs of individuals with pancreatic cancer and liver metastasis.
Clinical Trials for Pancreatic Cancer with Liver Metastasis
Clinical trials are research studies that aim to evaluate new treatments or procedures for medical conditions, including pancreatic cancer with liver metastasis. These trials offer individuals with advanced pancreatic cancer the opportunity to access experimental treatments and potentially benefit from the latest research advancements.
Experimental treatments tested in clinical trials may include targeted therapies, immunotherapy, or combination therapies that combine multiple treatments. By participating in a clinical trial, individuals with pancreatic cancer and liver metastasis can potentially access new and innovative treatments that are not yet widely available.
It is important to note that clinical trials have strict eligibility criteria that determine who can participate. Factors such as age, overall health, and cancer stage may impact a person’s eligibility. Before enrolling in a clinical trial, individuals should discuss the potential benefits and risks with their healthcare team.
Benefits of Participating in Clinical Trials
Participating in a clinical trial for pancreatic cancer with liver metastasis can have several potential benefits, including:
- Access to experimental treatments that are not yet widely available
- Potentially improved treatment outcomes and increased survival rates
- The opportunity to contribute to medical research and advance our understanding of pancreatic cancer and liver metastasis
Finding Clinical Trials for Pancreatic Cancer with Liver Metastasis
Individuals interested in participating in a clinical trial for pancreatic cancer with liver metastasis can speak with their healthcare team to learn about ongoing trials in their area. Additionally, websites such as ClinicalTrials.gov provide a comprehensive database of clinical trials for various medical conditions, including pancreatic cancer and liver metastasis.
Alternative and Complementary Therapies
While traditional medical treatments for pancreatic cancer with liver metastasis are essential, some individuals may consider alternative and complementary therapies to supplement their treatment plan. Alternative therapies include non-traditional medical interventions, such as herbal remedies or acupuncture. Complementary therapies, on the other hand, are used alongside traditional medical treatments to help manage symptoms and improve overall well-being.
Alternative Therapies
Alternative therapies aim to enhance the body’s natural healing abilities while minimizing the side effects of traditional treatments. Some options include:
| Therapy | Description |
|---|---|
| Herbal remedies | Herbs such as milk thistle, turmeric, and ginger are believed to have anti-inflammatory and antioxidant properties that may help reduce cancer-related symptoms. |
| Acupuncture | This traditional Chinese therapy involves the insertion of fine needles into specific points on the body to stimulate healing and reduce pain. |
| Mind-body therapies | Techniques such as meditation, yoga, and tai chi can help improve mental health and reduce stress, which may aid in cancer management. |
It’s important to discuss any alternative therapy with your healthcare professional before trying it, as some may interfere with traditional cancer treatments.
Complementary Therapies
Complementary therapies focus on enhancing an individual’s quality of life while undergoing traditional cancer treatment. They include:
- Aromatherapy
- Massage therapy
- Music therapy
- Art therapy
- Nutritional counseling to manage symptoms like appetite loss and nausea
Complementary therapies can provide emotional and psychological support, which may improve an individual’s overall well-being during cancer treatment. However, it’s crucial to talk to your healthcare professional before starting any complementary therapy, as some may not be appropriate for individuals with certain medical conditions or may interact with traditional cancer treatments.
Emotional Support and Psychosocial Care
Living with pancreatic cancer that has metastasized to the liver can be emotionally overwhelming for patients and their loved ones. Seeking emotional support and accessing psychosocial care services can help individuals cope with the physical, emotional, and practical challenges that come with the disease.
It is essential to have a supportive network to lean on during this difficult time. Family and friends can provide emotional support, while support groups can connect individuals with others who are going through similar experiences. Professional counseling can also be beneficial in managing stress, anxiety, and depression.
Psychosocial care services can also provide practical assistance, such as financial counseling and legal advice. These services can help reduce the stress of navigating the healthcare system and managing medical bills.
The Benefits of Emotional Support
Emotional support can improve the quality of life for patients and their loved ones. It can also help individuals cope with symptoms, side effects of treatment, and the stress of living with a chronic disease. Research has shown that individuals who receive emotional support have better coping skills, less anxiety and depression, and an overall better quality of life.
Psychosocial Care Services
Psychosocial care services offer a range of support to individuals with pancreatic cancer and their families. These services can help with financial and legal concerns, communication with healthcare providers, and care coordination. Additionally, some organizations offer assistance with transportation to medical appointments and help with household tasks.
| Psychosocial care services include: |
|---|
| Financial counseling |
| Legal advice |
| Care coordination |
| Transportation services |
| Assistance with household tasks |
Living with Pancreatic Cancer Spread to the Liver
Dealing with pancreatic cancer spread to the liver can be challenging, both physically and emotionally. Below are some practical tips and coping strategies to help individuals manage their symptoms and maintain a healthy lifestyle:
Managing Symptoms:
- Eat small, frequent meals to help manage digestive symptoms such as nausea and vomiting.
- Stay hydrated by drinking plenty of water and other fluids, especially if experiencing diarrhea or other gastrointestinal issues.
- Practice good oral hygiene to help prevent infections, which can be more common in individuals with compromised immune systems.
- Take medication as prescribed and communicate any concerns or side effects with healthcare professionals.
Maintaining a Healthy Lifestyle:
- Stay physically active as much as possible, even if it means taking short walks or doing light stretching exercises. Consult with a healthcare professional before starting any new exercise routine.
- Eat a balanced diet that is rich in fruits, vegetables, whole grains, and lean protein.
- Avoid smoking and excessive alcohol consumption, both of which can worsen symptoms and affect treatment outcomes.
- Get enough rest and consider incorporating relaxation techniques such as deep breathing exercises or meditation.
Accessing Support Resources:
Finally, it is important to seek emotional support and access psychosocial care services to help cope with the emotional impact of living with pancreatic cancer with liver metastasis:
- Join a support group of individuals who are going through a similar experience.
- Talk to a mental health professional who can provide guidance and support with coping strategies for the cancer diagnosis.
- Utilize complementary therapies like acupuncture or massage to help manage stress and physical symptoms.
By implementing these strategies, individuals with pancreatic cancer and liver metastasis can improve their quality of life and feel empowered in their cancer journey.
Research and Future Directions
The management of pancreatic cancer with liver metastasis is a complex challenge that requires a multidisciplinary approach. While progress has been made in recent years, there is still much to be done to improve outcomes for individuals affected by this disease.
Research efforts focused on pancreatic cancer and liver metastasis are ongoing, to develop new and innovative treatments. Advances in technology such as precision medicine, immunotherapy, and gene editing hold promise for improving outcomes.
One area of focus in pancreatic cancer research is the development of targeted therapies that aim to inhibit specific molecular targets. These therapies have shown some promise in clinical trials, and more research is ongoing to identify new targets.
Another area of interest is immunotherapy, which uses the body’s immune system to target cancer cells. Checkpoint inhibitors, a type of immunotherapy, have shown some promise in clinical trials, and researchers are exploring ways to enhance their effectiveness.
Clinical trials are also ongoing to test experimental treatments for pancreatic cancer with liver metastasis. These trials aim to evaluate the safety and effectiveness of novel therapies, and individuals affected by pancreatic cancer may be eligible to participate.
As research into pancreatic cancer and liver metastasis advances, the hope is to develop new and effective treatments that improve survival rates and quality of life for those affected by this disease.
FAQ
What is pancreatic cancer?
Pancreatic cancer is a type of cancer that originates in the pancreas, a gland located behind the stomach. It is considered one of the most aggressive forms of cancer, as it often spreads quickly to other organs, including the liver.
What are the risk factors for pancreatic cancer?
Several risk factors increase the likelihood of developing pancreatic cancer, including smoking, obesity, family history of the disease, age (typically over 60 years old), and certain genetic conditions.
What are the symptoms of pancreatic cancer?
The symptoms of pancreatic cancer can vary, but common signs include abdominal pain, jaundice (yellowing of the skin and eyes), unexplained weight loss, loss of appetite, and changes in stool consistency.
What is liver metastasis?
Liver metastasis refers to the spread of cancer from its original site to the liver. In the case of pancreatic cancer, it means that cancer cells from the pancreas have migrated and formed tumors in the liver.
How does pancreatic cancer spread to the liver?
Pancreatic cancer can spread to the liver through the bloodstream or the lymphatic system. Cancer cells can invade nearby blood vessels or lymph nodes, allowing them to reach the liver and form metastatic tumors.
What is the prognosis for pancreatic cancer with liver metastasis?
The prognosis for pancreatic cancer with liver metastasis is generally poor. The overall survival rates are lower compared to pancreatic cancer without liver involvement. However, every case is unique, and survival time can vary depending on factors such as the stage of cancer and the individual’s overall health.
What factors influence survival time in pancreatic cancer with liver metastasis?
Survival time in pancreatic cancer with liver metastasis can be influenced by various factors, including the stage of cancer at diagnosis, the extent of liver involvement, the individual’s response to treatment, overall health condition, and genetic factors.
What are the treatment options for pancreatic cancer spread to the liver?
Treatment options for pancreatic cancer with liver metastasis may include surgery, chemotherapy, targeted therapy, immunotherapy, palliative care, and participation in clinical trials. The choice of treatment depends on several factors, including the stage of cancer and the individual’s overall health.
Can surgical interventions be used to treat liver metastasis in pancreatic cancer?
Yes, surgical interventions can be used to treat liver metastasis in pancreatic cancer. Techniques such as resection (removal of the affected part of the liver) and ablation (destruction of tumors using extreme heat or cold) may be employed, depending on the individual’s specific case.
What role does chemotherapy play in managing pancreatic cancer with liver metastasis?
Chemotherapy plays a crucial role in managing pancreatic cancer with liver metastasis. It involves the use of drugs that can kill cancer cells or slow down their growth. Different chemotherapy drugs or combinations of drugs may be prescribed, depending on the individual’s condition.
What is targeted therapy, and how is it used in treating pancreatic cancer with liver metastasis?
Targeted therapy is a treatment approach that aims to target specific molecular targets in cancer cells. In pancreatic cancer with liver metastasis, targeted therapies may be used to inhibit certain molecules or pathways involved in cancer growth. These therapies are often used in combination with other treatments.
Are there any advancements in immunotherapy for pancreatic cancer with liver metastasis?
Yes, there have been advancements in immunotherapy for pancreatic cancer with liver metastasis. Immunotherapy utilizes drugs called checkpoint inhibitors to enhance the immune system’s response against cancer cells. Clinical trials are ongoing to evaluate the effectiveness of immunotherapy in managing this condition.
How can palliative care and supportive treatments help individuals with pancreatic cancer and liver metastasis?
Palliative care and supportive treatments aim to improve the quality of life for individuals living with pancreatic cancer and liver metastasis. These therapies focus on managing symptoms, providing psychological support, and addressing the physical and emotional needs of patients and their families.
Are there any clinical trials available for individuals with pancreatic cancer and liver metastasis?
Yes, there are clinical trials available for individuals with pancreatic cancer and liver metastasis. Clinical trials offer access to experimental treatments and allow individuals to contribute to medical research and potentially benefit from advancements in the field.
What alternative and complementary therapies are commonly considered for pancreatic cancer with liver metastasis?
Some individuals consider alternative and complementary therapies alongside conventional treatments for pancreatic cancer with liver metastasis. These may include acupuncture, herbal remedies, nutrition therapy, and mind-body techniques. It is crucial to discuss these options with healthcare professionals.
How can emotional support and psychosocial care benefit individuals with pancreatic cancer and liver metastasis?
Emotional support and psychosocial care play a significant role in the well-being of individuals with pancreatic cancer and liver metastasis. They can help individuals cope with the emotional challenges of the disease, provide resources for managing stress, and offer guidance for navigating the healthcare system.
What are some practical tips for living with pancreatic cancer spread to the liver?
Living with pancreatic cancer and liver metastasis can be challenging, but there are practical tips that can help. These include maintaining a healthy lifestyle, managing symptoms effectively, seeking support from loved ones, staying informed about treatment options, and utilizing support resources such as patient advocacy groups.
What research efforts are underway to improve outcomes for pancreatic cancer with liver metastasis?
There are ongoing research efforts aimed at improving outcomes for individuals with pancreatic cancer and liver metastasis. These studies focus on developing new treatments, identifying biomarkers for early detection, understanding the molecular mechanisms of cancer progression, and exploring novel therapeutic targets.