Histiocytic Lymphoma: Understanding This Rare Cancer
Stagescancer.net - Delving into the realm of rare cancers, histiocytic lymphoma emerges as a confounding adversary within the spectrum of histiocytic disorders. The complexity of this immune system malignancy presents a formidable challenge for patients and healthcare professionals alike. Cultivating lymphoma awareness is pivotal for forging pathways to early detection and facilitating advanced lymphoma treatment options. This introductory exploration aims to shed light on histiocytic lymphoma, fostering a deeper comprehension of its impact and the ongoing efforts to combat it.
Introduction to Histiocytic Lymphoma
Delving into the complexities of histiocytic neoplasms, we uncover the multi-faceted world of histiocytic lymphoma—a rare and often misunderstood cancer impacting the lymphatic system's histiocyte cells. Despite its low incidence rate, understanding this condition remains a pivotal aspect of healthcare awareness. Intractable challenges pervade the journey from accurate cancer diagnosis to effective treatment, as the subdued awareness hinders early detection—a critical juncture for improving patient outcomes.
What Is Histiocytic Lymphoma?
At its core, histiocytic lymphoma is a malignancy of the lymphatic system, specifically targeting histiocytes. These cells, imperative to the immune system, can give rise to tumors that disrupt normal bodily functions and present an array of clinical manifestations. Although this disease falls under the wider category of lymphoproliferative disorders, its rarity and unique pathophysiology set it apart, necessitating bespoke clinical expertise and management strategies.
The Rarity and Importance of Awareness
The enigma that is histiocytic lymphoma evokes pressing questions about its rarity and the consequential impact on awareness. Unlike more prevalent cancers, the limited occurrences of this lymphoma type stunt widespread knowledge within both the general public and medical communities. Elevating consciousness about histiocytic neoplasms, therefore, is not merely an educational endeavor but a lifesaving initiative to propel earlier intervention and enhance patient prognoses.
| Disease Type | Incidence Rate | Affected Cell Type | Key Challenges |
|---|---|---|---|
| Histiocytic Lymphoma | Rare | Histiocytes of the Lymphatic System | Early Detection, Specialized Treatment |
| Common Lymphomas | More Common | Lymphocytes (B-cells and T-cells) | General Awareness, Broad Treatment Protocols |
With fervent efforts towards boosting healthcare awareness, particularly in the realm of rare malignancies such as histiocytic lymphoma, the goal remains clear: to demystify the nuances of such diseases, thereby fostering an environment ripe for early diagnosis and treatment excellence.
Identifying Histiocytic Lymphoma Symptoms
Being vigilant about the cancer symptoms and lymphoma signs can significantly contribute to early detection and effective management of histiocytic lymphoma. Individuals must be educated on the nuances of these symptoms to seek medical consultation promptly.
Common Signs of Histiocytic Lymphoma
The manifestation of histiocytic lymphoma can vary from person to person, but there are several common indicators to watch for. Proactive health monitoring can lead to the early identification of symptoms, which is essential for improving the likelihood of successful treatment outcomes.
- Swollen lymph nodes, often in the neck, armpits, or groin
- Persistent fatigue that isn't alleviated by rest
- Unexplained weight loss without changes in diet or exercise habits
- Fevers with no apparent cause
When to Seek Medical Advice
Recognizing when to consult a healthcare provider can be the turning point in the fight against histiocytic lymphoma. If you or your loved ones experience any combination of the symptoms listed above, it is imperative to arrange for a medical examination.
- Notice persistent swelling of lymph nodes, particularly if the swelling is painless
- Experience unexplained fever and night sweats over some time
- Observe dramatic weight loss that cannot be attributed to lifestyle changes
- Feel a prolonged sense of fatigue that disrupts daily activities
Causes and Risk Factors Associated with Histiocytic Lymphoma
Understanding the intricacies of oncogenesis is crucial when exploring the nuances of histiocytic lymphoma. A comprehensive risk factor analysis reveals a complex interplay between genetic, environmental, and lifestyle elements that contribute to the cancer etiology. Research continuously probes the depths of these associations, endeavoring to elucidate the disease's origins and identify populations at higher risk due to immune system disorders and other predisposing conditions.
- Genetic predispositions in familial clusters
- Environmental exposures to carcinogens
- Lifestyle factors, such as diet and exercise
- The existing immune system compromises
Below is an examination of the risk factors known to increase the propensity for developing histiocytic lymphoma:
| Risk Factor | Description | Impact on Oncogenesis |
|---|---|---|
| Genetic Mutations | Hereditary or acquired genetic anomalies | May drive abnormal cell growth leading to malignancy |
| Environmental Toxins | Exposure to substances known to be carcinogenic | Can contribute to cell DNA damage and cancer development |
| Lifestyle Factors | Behaviors such as smoking and prolonged UV exposure | May significantly elevate the risk of lymphoma |
| Autoimmune Conditions | Disorders causing chronic immune system activation | Possibly increases vulnerability to lymphocyte transformation |
The confluence of these factors underscores the disease's complexity, as it straddles the junction between inherent susceptibilities and external provocations. Continuous investigation in the field of cancer etiology and immune system disorders provides invaluable insights, informing preventative strategies and aiding in tailoring personalized approaches to diagnosis and treatment.
Diagnostic Procedures for Histiocytic Lymphoma
Accurate diagnosis is a critical step in the effective management of histiocytic lymphoma. The journey to a conclusive diagnosis begins with an array of investigative procedures that provide healthcare professionals with the necessary insights to identify this malignancy.
Initial Screening and Patient History
Taking a comprehensive patient history is paramount, as it reveals potential symptoms and risk factors associated with lymphoma. Initial screenings may incorporate physical examinations to detect signs like swollen lymph nodes, which often prompt further testing.
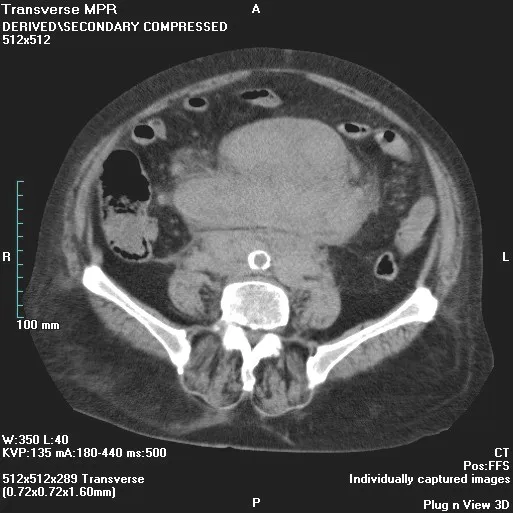
Advanced Diagnostic Imaging and Biopsy
For more definitive lymphoma diagnosis, healthcare providers rely on sophisticated imaging techniques coupled with biopsy procedures. Imaging such as CT scans, MRIs, and PET scans play an indispensable role by offering a detailed internal view, which helps in identifying the extent of the disease.
Biopsies, including excisional or needle biopsies, are essential for obtaining tissue samples that confirm the presence of lymphoma through histopathological examination. Here's an overview of commonly used diagnostic tools:
| Diagnostic Tool | Usage | Benefit |
|---|---|---|
| Physical Examination | Initial assessment of symptoms | Identifies superficial signs of disease |
| Complete Blood Count (CBC) | Evaluate overall health and detect blood disorders | Provides a quick, comprehensive overview of blood cell levels |
| CT Scan | Detailed cross-sectional images of the body | Assists in determining the stage of lymphoma |
| MRI | Detailed images using magnetism and radio waves | Useful for imaging soft tissues and the central nervous system |
| PET Scan | Displays metabolic activity of cells | Detects the aggressiveness and spread of cancer cells |
| Biopsy | Extraction of tissue sample for examination | Confirms the diagnosis of lymphoma |
Following these diagnostic steps, healthcare providers analyze the gathered data to characterize the nature of the lymphoma, which is crucial for planning an appropriate course of treatment.
Histiocytic Lymphoma
With varied presentations and prognoses, histiocytic lymphoma requires meticulous classification to guide treatment and predict outcomes. Exploring the types, classifications, and intricate pathophysiology of cancer unveils the complexities of these hematologic malignancies and informs medical practice.
Histiocytic Lymphoma Types and Classifications
As a subtype of lymphoma, histiocytic lymphoma is categorized based on specific characteristics such as cellular morphology and genetic markers, which play critical roles in understanding the disease. Below is a comprehensive table outlining the prevalent types and classifications used in clinical settings:
| Type | Morphology | Genetic Markers | Clinical Behavior |
|---|---|---|---|
| Classical Histiocytic Lymphoma | Large histiocytic cells with prominent nucleoli | BRAF mutations | Aggressive, rapid progression |
| Indeterminate Dendritic Cell Tumor | Oval-shaped indeterminate cells | FLT3 and KRAS mutations | Localized or systemic spread with variable outcomes |
| Erdheim-Chester Disease | Foamy histiocytes, Touton giant cells | PIK3CA, NRAS mutations | Multi-system involvement, chronic course |
| Rosai-Dorfman Disease | Large S100-positive histiocytes with emperipolesis | Mutation in SLC29A3 | Typically nodal, can have extranodal manifestations |
| Langerhans Cell Histiocytosis | Birbeck granules, 'coffee bean' nuclei | BRAF V600E mutations | Potential for skin lesions, bone involvement, and pituitary gland dysfunction |
Understanding the Pathophysiology
The pathophysiology of cancer within histiocytic lymphoma is rooted in the abnormal proliferation of histiocytes and their precursors. Such disruptions often result from complex genetic alterations that induce uncontrolled cell growth. By dissecting the disease's pathophysiology, researchers and clinicians alike seek to develop targeted therapies that more effectively interrupt the disease's course, aiming for improved patient survival and quality of life.
Differentiating Histiocytic Lymphoma From Other Hematologic Malignancies
The accurate diagnosis of histiocytic lymphoma necessitates a meticulous differential diagnosis process, as it shares overlapping symptoms with several other hematological disorders. Blood cancers, particularly, present a unique challenge for healthcare professionals who are tasked with distinguishing between various malignancies that exhibit similar clinical manifestations. The identification of specific diagnostic biomarkers is therefore critical in confirming histiocytic lymphoma and directing appropriate treatment.
Comparative Symptomatology
While swollen lymph nodes, fever, and fatigue are indications commonly found in many blood cancers, there are nuanced differences in symptom presentation that can steer a differential diagnosis toward histiocytic lymphoma. For instance, the skin lesions and distinct histological findings are more suggestive of histiocytic disorders. However, a thorough evaluation of symptoms in the context of each patient's clinical profile remains vital in narrowing the diagnostic considerations.
Unique Markers and Diagnostic Challenges
Identifying unique diagnostic biomarkers plays a fundamental role in differentiating histiocytic lymphoma from other hematological malignancies. Advanced immunophenotyping and genetic testing have emerged as pivotal tools in the detection of specific markers indicative of histiocytic lymphoma. Yet, the variability of these markers and their expression across different cases can introduce significant diagnostic challenges, underpinning the importance of combined clinical, histological, and molecular analyses.
| Hematologic Malignancy | Common Symptoms | Diagnostic Biomarkers | Distinguishing Features |
|---|---|---|---|
| Histiocytic Lymphoma | Swollen lymph nodes, skin lesions, hepatosplenomegaly | CD163, CD68, Langerin | Histiocyte proliferation, Multisystemic involvement |
| Acute Lymphoblastic Leukemia (ALL) | Fatigue, fever, bone pain, bruising | TDT, CD10, CD19, CD22 | Precursor B or T lymphoblasts in bone marrow |
| Chronic Myelogenous Leukemia (CML) | Weakness, fatigue, night sweats, splenomegaly | BCR-ABL1 fusion gene | Presence of Philadelphia chromosome, myeloid cell proliferation |
| Non-Hodgkin Lymphoma (NHL) | Swollen lymph nodes, abdominal pain, chest pain | CD20, CD3, CD5, BCL2 | B-cell or T-cell lineage, lymph node architecture disruption |
| Hodgkin Lymphoma (HL) | Swollen lymph nodes, persistent fatigue, itching | CD15, CD30, Epstein-Barr virus | Reed-Sternberg cells, nodular lymphocyte predominance |
With an enhanced understanding of the nuances and complexities involved in the accurate diagnosis of histiocytic lymphoma and other hematological disorders, healthcare professionals can move towards more targeted and individualized treatment approaches, significantly impacting the outcomes for patients facing these challenging diagnoses.
The Role of Genetics in Histiocytic Lymphoma
Investigating the influence of genetic markers on histiocytic lymphoma uncovers the inextricable connection between our DNA and this immune system malignancy. Genomic research has begun to illuminate specific mutations that may contribute to oncogenesis, fostering a better understanding of genetic predisposition and its relationship with hereditary cancers. Notably, advancements in oncogenetics are revolutionizing the identification of individuals at increased risk for cancers, including rare lymphomas.
Modern studies focus on distinguishing the genetic signatures that are indicative of a predisposition to histiocytic lymphoma. The identification of these genetic markers not only enhances diagnostic precision but also opens avenues for targeted therapy. Genomic profiling continues to reveal complexities within hereditary links, providing deeper insights into the mechanisms through which genetic factors trigger the pathological processes underlying this disease.
Below is a detailed comparison of known genetic markers associated with histiocytic lymphoma and their potential implications:
| Genetic Marker | Association with Histiocytic Lymphoma | Potential Clinical Implication |
|---|---|---|
| BRAF V600E | Commonly found in Langerhans Cell Histiocytosis, a form of histiocytic lymphoma | Target for therapies using BRAF inhibitors |
| MAP2K1 | Mutation associated with histiocytic disorders | May influence the response to MEK inhibitors |
| TP53 | Abnormalities linked to various cancers, including hematologic malignancies | Indicative of disease prognosis and therapeutic response |
While the presence of genetic predisposition does not necessarily mean an individual will develop histiocytic lymphoma, it does signify a heightened need for vigilance and potentially more frequent screening for those with a family history of hereditary cancers. As the interplay between genetics and cancer becomes clearer, personalized medicine is poised to deliver treatments tailored to an individual's genetic profile, maximizing therapeutic efficacy while minimizing undue side effects.
Treatment Options for Histiocytic Lymphoma
Embarking on a treatment journey for histiocytic lymphoma involves understanding a multifaceted range of therapy options. With advancements in medicine, patients have access to both time-tested treatments and innovative therapies that are currently being explored in clinical trials. The aim is to provide a personalized treatment plan suited to the specificities of each patient's condition.
Conventional Therapies for Management
Standard cancer treatment protocols for histiocytic lymphoma typically include chemotherapy and radiation therapy. These treatments have been the cornerstone of care, with their potential to significantly reduce tumor burden and manage symptoms. The protocols and drug regimens vary depending on the stage and aggressiveness of the disease.
- Chemotherapy: Utilizing cytotoxic drugs to kill rapidly dividing cancer cells.
- Radiation Therapy: Targeting cancerous cells with high-energy particles or waves to destroy or damage them.
Emerging Treatments and Clinical Trials
Research in the field of oncology is dynamic, with targeted therapy and participation in clinical trials representing the frontier of innovative cancer treatment procedures. These novel approaches aim to target cancer cells more precisely and with fewer side effects than conventional treatments.
| Treatment Modality | Objective | Key Benefits |
|---|---|---|
| Targeted Therapy | Focus on specific molecular targets associated with cancer | Higher precision, fewer off-target effects |
| Immunotherapy | Boost the body's immune response against cancer cells | Can offer durable responses in some patients |
| Clinical Trials | Test emerging therapies and new drug combinations | Access to cutting-edge treatment options |
Participation in clinical trials can offer access to novel treatments that are not yet available to the public. These studies are critical for the development of new therapies and for gaining insights into the effectiveness and safety of experimental approaches. Patients considering clinical trials should discuss the potential risks and benefits with their healthcare provider.
Predicting and Improving Prognosis
The trajectory of histiocytic lymphoma, a formidable opponent in the oncological landscape, hinges on stringent prognostic evaluations. A myriad of factors coalesce to sketch the outline of cancer prognosis, painting a picture that varies from patient to patient. Variables such as disease stage, patient age, and the body's response to treatment are some of the prognostic factors that are carefully analyzed to weave an accurate prognosis tapestry. In this landscape, survival rate and treatment outcomes serve as key signposts, guiding patients and healthcare professionals through the maze of therapeutic decisions and expectations.
Factors Influencing Outcome
To distill the essence of personalized Medicare, clinicians articulate an in-depth discourse on the diverse factors that sculpt the treatment outcomes. Not merely limited to the clinical presentation, these elements encompass a spectrum of biological, physiological, and therapeutic touchpoints. Each factor is a cog in the complex machinery of prognosis, with the potential to alter the survival rate either singularly or in concert with others. For instance, the aggressive nature of advanced-stage lymphoma can tarnish the prognosis, while an early-stage detection could imbue the forecast with optimism.
- Disease Stage: The extent to which the lymphoma has proliferated throughout the body.
- Patient Age: Younger patients often have a more robust prognosis, but age alone isn't a definitive predictor.
- Treatment Response: The efficacy of treatments such as chemotherapy, can significantly influence remission rates.
- Patient's Overall Health: Factors including preexisting conditions that may impact the ability to withstand aggressive treatments.
Advancements in Prognostic Tools
As science surges forward, the arsenal of prognostic tools sees an infusion of sophisticated technologies. Medical advancements have introduced innovative methodologies for enhanced precision in predicting cancer prognosis. This not only benefits patients through personalized treatment plans but also opens new vistas in understanding the disease's trajectory. Data analytics, biomarker research, and imaging innovations constitute the forefront of these prognostic advancements.
| Prognostic Tool | Function | Impact on Prognosis |
|---|---|---|
| Genetic Profiling | Identifies individual genetic mutations associated with the cancer. | Tailor therapy targets specific cellular abnormalities, potentially improving survival rates. |
| Molecular Imaging | Provides detailed images of the tumor's molecular structure. | Enables early detection of metastasis and helps in assessing treatment response. |
| Biomarker Testing | Examines the presence of specific proteins or genes that signify the cancer's behavior. | Facilitates more accurate predictions of disease progression and treatment outcomes. |
| Artificial Intelligence (AI) | Analyses massive datasets to uncover patterns and predictions not easily discernible by humans. | Refines prognostic accuracy, potentially revealing new prognostic factors. |
In closing, the interplay of prognostic factors and the continual evolution of prognostic tools provide a dual framework for anticipating the course of histiocytic lymphoma. By harnessing these insights, the pursuit of extending survival rates and enhancing the quality of life for patients continues with renewed vigor.
Living with Histiocytic Lymphoma
Facing a diagnosis of histiocytic lymphoma is a profound challenge that requires not just medical intervention but a robust support system for the patient. Managing the cancer journey and the treatment side effects must go hand in hand with enhancing the quality of life. In this phase, patient support becomes a cornerstone of care, and navigating the landscape of this disease calls for a comprehensive approach.
Coping with the Diagnosis
The initial diagnosis of histiocytic lymphoma can often leave patients and their families feeling overwhelmed. Emotional support is crucial during this time, and seeking counseling or joining a support group can be instrumental in maintaining a positive outlook. Strategies for coping might include establishing open communication with healthcare professionals and creating a support network comprising friends, family, and fellow patients.
Navigating Treatment and its Side Effects
As patients embark on their treatment regimen, managing side effects is a priority to ensure they maintain as much normality in their lives as possible. Treatments for histiocytic lymphoma, while life-saving, often come with a host of challenging side effects ranging from fatigue to more severe complications.
- Stay informed: Understanding the potential side effects of treatments like chemotherapy, radiation, or targeted therapy can empower patients to prepare and address them proactively.
- Regular monitoring: Keeping track of side effects and communicating them to the medical team allows for timely management and, if necessary, treatment adjustment.
- Seeking specialized care: Certain side effects may require the expertise of specialists, such as dietitians or physiotherapists, to provide targeted support and improve outcomes.
Below is a brief overview of common side effects and suggested management strategies:
| Treatment Side Effect | Management Strategy | Supportive Care Needed |
|---|---|---|
| Fatigue | Regular mild exercise and adequate rest | A physical therapist for an exercise plan |
| Nausea | Anti-emetic medications and proper hydration | A dietitian to help with meal planning |
| Neuropathy | Maintenance of blood sugar levels, medications | Neurologist for ongoing care |
| Hair Loss | Scalp cooling techniques | Support groups for emotional impact |
| Infection Risk | Good hygiene and avoiding exposure | Infection disease specialist for preventive advice |
Support Systems and Resources for Histiocytic Lymphoma Patients
Embarking on the journey of battling histiocytic lymphoma, patients and their families need not face the challenges alone. A myriad of support systems exist, designed to provide comfort, knowledge, and empowerment to those affected by this condition. By tapping into these resources, individuals can find not only solace but also practical assistance tailored to their unique needs.
Role of Support Groups and Counseling
Joining a cancer support group can significantly impact one's emotional well-being. These groups provide a safe environment where experiences and feelings can be shared without judgment. For personalized guidance, healthcare counseling services are also available, offering professional advice and coping strategies to manage the psychological stresses of cancer diagnosis and treatment.
Accessing Reliable Information and Assistance
The journey to accessing reliable patient resources begins with educating oneself through reputable organizations and health centers. Financial and healthcare assistance programs work to alleviate the burden of treatment costs, providing aid in a structured and compassionate manner. Utilizing these resources can pave the way toward more manageable care and improved quality of life.
- Local healthcare facilities and cancer centers often have resource offices
- Non-profit organizations dedicated to cancer care typically offer a range of support services
- Online platforms can provide current information and virtual support communities
Current Research and Developments in Histiocytic Lymphoma Care
The realm of histiocytic lymphoma treatment and management is witnessing significant strides through dedicated oncology research. Cancer care innovation is pivotal in shaping the future of therapy for this rare consternation. The relentless pursuit of knowledge is yielding therapeutic research that is not only broadening the spectrum of viable treatments but also enhancing the precision and effectiveness of each intervention.
Investigating New Therapeutic Approaches
New therapeutic approaches are being investigated to improve outcomes for those battling histiocytic lymphoma. Breakthroughs in targeted therapy, immunotherapy, and personalized medicine are at the forefront, offering hope through treatments that are designed to be more efficient and less toxic than conventional methods. These investigative therapies hold the promise of transforming the standards of care, working to extend survival rates, and ultimately aiming for eradication of the disease.
The Importance of Research Participation
Patient participation plays a critical role in the progress of medical research. By engaging in clinical trials, patients contribute to the collective understanding of histiocytic lymphoma, directly influencing the advancement of new treatments and enhancing the quality of care for future generations. This collaborative approach between patients and researchers is a cornerstone of medical achievement and is essential for delivering the next wave of groundbreaking cancer care innovations.
FAQ
What is Histiocytic Lymphoma?
Histiocytic Lymphoma is a rare type of cancer that originates in the body's immune system cells known as histiocytes. These cells are part of the body's defense against infections and diseases, but in histiocytic lymphoma, they become cancerous and can cause damage to the lymphatic system as well as other organs.
Why is it important to raise awareness about Histiocytic Lymphoma?
Raising awareness about Histiocytic Lymphoma is critical because its rarity often leads to delayed diagnosis and treatment. Increased awareness among healthcare professionals and the public can lead to earlier detection, more effective management, and ultimately better outcomes for patients.
What are common signs of Histiocytic Lymphoma to look out for?
Common signs of Histiocytic Lymphoma include swollen lymph nodes, persistent fatigue, unexplained weight loss, fever, and night sweats. It is essential for individuals experiencing these symptoms to seek medical advice as they may indicate the presence of this lymphoproliferative disorder.
What causes Histiocytic Lymphoma?
The exact causes of Histiocytic Lymphoma are not entirely understood. Some research suggests a combination of genetic, environmental, and lifestyle factors could contribute to its development. Ongoing research strives to pinpoint specific causes and risk factors associated with this immune system malignancy.
How is Histiocytic Lymphoma diagnosed?
Diagnosis of Histiocytic Lymphoma typically involves a series of steps beginning with patient history and physical examination. This is followed by advanced diagnostic imaging such as CT scans, MRIs, or PET scans, and confirmation with a biopsy procedure where a sample of affected tissue is examined for cancer cells.
Are there different types of Histiocytic Lymphoma?
Yes, Histiocytic Lymphoma can be classified into various types based on cellular morphology, genetic markers, and clinical behavior. Understanding these classifications helps in determining appropriate treatment plans.
How is Histiocytic Lymphoma different from other hematologic malignancies?
Histiocytic Lymphoma is unique due to its origin from histiocytes and may present with different symptoms and diagnostic markers compared to other blood cancers. Distinctions in symptomatology and cellular markers are fundamental for differential diagnosis.
What role do genetics play in Histiocytic Lymphoma?
Genetics may play a role in the development and progression of Histiocytic Lymphoma. Specific genetic markers and a possible hereditary predisposition are areas of active research, contributing to a better understanding of the disease and the development of targeted treatments.
What are the treatment options currently available for Histiocytic Lymphoma?
Treatment for Histiocytic Lymphoma may include conventional therapies such as chemotherapy and radiation therapy. Additionally, there are targeted therapies and ongoing clinical trials exploring novel treatments aimed at improving patient outcomes.
How can the prognosis of Histiocytic Lymphoma be improved?
Prognosis can be influenced by several factors including the stage of the disease, the patient's age, and response to treatment. Advancements in prognostic tools and personalized treatment have the potential to better predict outcomes and improve the prognosis for patients with Histiocytic Lymphoma.
How do patients cope with a Histiocytic Lymphoma diagnosis?
Coping with a Histiocytic Lymphoma diagnosis requires a robust support system, including counseling, patient support groups, and educational resources. Strategies may include managing treatment side effects, maintaining mental and emotional health, and seeking assistance from healthcare professionals.
What kinds of support systems are available for Histiocytic Lymphoma patients?
There are various support systems available, including support groups, counseling services, and assistance programs that offer financial and healthcare guidance. Access to reliable information and resources is vital for patients and their families throughout the cancer journey.
How does current research and development affect the care of Histiocytic Lymphoma patients?
Current research and development are crucial for creating new therapeutic approaches for Histiocytic Lymphoma, including advancements in genetic analysis, drug development, and clinical trials. Patient participation in research is essential for pushing the boundaries of current treatment standards and improving future care.