PD-L1 Lung Cancer: Diagnosis, Prognostic, Immunotherapy
Stagescancer.net - PD-L1, or programmed death-ligand 1, has emerged as a key player in the field of lung cancer research. This protein, expressed on both tumor cells and immune cells, plays a critical role in the interaction between the immune system and lung cancer cells.
In this article, we will explore the significance of PD-L1 in lung cancer diagnosis and treatment options, with a focus on improving patient outcomes. We will delve into the understanding of PD-L1 expression, discussing its implications for the immune system and tumor cells. Subsequently, we will explore the methods used for diagnosing PD-L1 in lung cancer, including biopsy, immunohistochemistry, and other diagnostic tests.
PD-L1 also serves as a valuable prognostic marker in lung cancer, providing valuable insights into patient prognosis. Additionally, we will discuss the role of immunotherapy in targeting PD-L1, highlighting the use of checkpoint inhibitors and their mechanism of action.
This article will also shed light on ongoing clinical trials that explore the efficacy of PD-L1 inhibitors in lung cancer treatment, giving readers insights into the latest advancements and treatment strategies. Furthermore, we will discuss the potential benefits of combining PD-L1 inhibitors with other treatment modalities such as chemotherapy, targeted therapy, or radiation therapy.
While PD-L1 inhibitors have shown promising results, their use is not without potential immune-related adverse events. We will examine the possible side effects associated with PD-L1 inhibitors and underline the importance of monitoring and managing these adverse events in lung cancer patients.
Moreover, this article will provide an overview of the current guidelines for PD-L1 testing in lung cancer, emphasizing the importance of standardized biomarker testing protocols. We will also delve into the mechanisms by which lung cancer cells develop resistance to PD-L1 inhibitors, allowing for a better understanding of immune escape strategies.
As we look to the future, we will explore the potential directions of PD-L1 research in lung cancer, highlighting emerging therapeutic advancements and areas of investigation. Additionally, we will discuss the role of PD-L1 biomarkers in personalized medicine for lung cancer patients, showcasing how this information can be used to tailor treatment plans.
Supportive care is vital for PD-L1 lung cancer patients, and we will emphasize the importance of proper symptom management and improving their quality of life. Lastly, we will highlight the notable research organizations and advocacy groups dedicated to PD-L1 lung cancer research, fostering collaboration among the scientific community.
In conclusion, this article aims to provide a comprehensive overview of PD-L1 in lung cancer, emphasizing the critical role it plays in diagnosis and treatment options. By staying informed about the latest advancements and research, we can pave the way for better patient outcomes and contribute to the progress in the fight against lung cancer.
Understanding PD-L1 Expression
In lung cancer, PD-L1 expression plays a crucial role in the interaction between the immune system and tumor cells. PD-L1, also known as programmed death-ligand 1, is a protein that is found on the surface of certain cells, including tumor cells in the lungs. When PD-L1 interacts with its receptor PD-1 on immune cells, it can inhibit the immune system's response against the tumor.
The expression of PD-L1 can be influenced by various factors, including genetic mutations, inflammatory signals, and tumor microenvironment. High levels of PD-L1 expression in lung cancer are associated with immune evasion, allowing tumor cells to evade detection and destruction by immune cells.
Research has shown that PD-L1 expression is not uniform across all lung cancer patients. The level of PD-L1 expression can vary within the tumor itself and between different patients.
Role of PD-L1 Expression in Immune Evasion
PD-L1 expression in lung cancer cells enables immune evasion through the PD-1/PD-L1 pathway. When PD-L1 on tumor cells interacts with PD-1 on immune cells, it sends inhibitory signals that suppress the immune system's ability to attack the tumor. This mechanism allows tumor cells to escape immune surveillance and continue to grow and spread.
Implications for Treatment and Prognosis
The level of PD-L1 expression in lung cancer cells has significant implications for treatment decisions and patient prognosis. High levels of PD-L1 expression have been associated with favorable responses to immunotherapy drugs called PD-L1 inhibitors or checkpoint inhibitors. These drugs block the interaction between PD-L1 and PD-1, allowing the immune system to mount a robust anti-tumor response.
A comprehensive understanding of PD-L1 expression in lung cancer is essential for identifying patients who might benefit from PD-L1 inhibitor therapy and predicting treatment outcomes. PD-L1 testing is now routinely performed in clinical practice to guide treatment decisions and personalize lung cancer therapy.
| PD-L1 Expression Level | Treatment Implications |
|---|---|
| High PD-L1 Expression | Potential response to PD-L1 inhibitors |
| Low PD-L1 Expression | Other treatment options may be considered |
| No PD-L1 Expression | Alternative treatment strategies required |
Table: Treatment implications based on PD-L1 expression level in lung cancer cells.
PD-L1 Diagnosis in Lung Cancer
Diagnosing PD-L1 in lung cancer involves various methods, including biopsy, immunohistochemistry, and diagnostic tests. These techniques play a crucial role in determining the PD-L1 expression levels and guiding treatment decisions.
Biopsy
A biopsy is commonly performed to obtain tissue samples for PD-L1 analysis. During a biopsy, a small piece of lung tissue is extracted and examined for the presence of PD-L1. This procedure helps in confirming the diagnosis of lung cancer and assessing the PD-L1 expression, which is important for determining the eligibility for immunotherapy.
Immunohistochemistry
Immunohistochemistry (IHC) is a commonly used technique to assess PD-L1 expression levels in lung cancer tissue samples obtained through biopsies. It involves staining the tissue samples with specific antibodies that bind to PD-L1, allowing for visual identification of PD-L1-positive tumor cells using a microscope. This method provides valuable information about the percentage of tumor cells expressing PD-L1, which helps in predicting the response to PD-L1 inhibitors.
Diagnostic Tests
In addition to biopsy and immunohistochemistry, various diagnostic tests are available to evaluate PD-L1 expression in lung cancer. These tests can be performed using different technologies, such as polymerase chain reaction (PCR) or next-generation sequencing (NGS), to detect specific genetic alterations or gene expression patterns associated with PD-L1. These diagnostic tests provide additional insights into the PD-L1 status and can help in tailoring personalized treatment options.
| Diagnostic Method | Advantages | Limitations |
|---|---|---|
| Biopsy | - Confirms the diagnosis of lung cancer- Provides tissue samples for PD-L1 analysis | - Invasive procedure- Limited sample availability- Potential risks and complications |
| Immunohistochemistry | - Visual identification of PD-L1 expression in tumor cells- Predicts response to PD-L1 inhibitors | - Requires skilled interpretation- Subject to inter-observer variability- Limited standardization across laboratories |
| Diagnostic Tests | - Detect specific genetic alterations or gene expression patterns- Provides additional insights into PD-L1 status | - High cost- Variable sensitivity and specificity |
PD-L1 as a Prognostic Marker
In the field of lung cancer, the role of PD-L1 as a prognostic marker has gained significant attention. PD-L1, also known as programmed death-ligand 1, is a protein expressed on the surface of tumor cells that plays a crucial role in suppressing the body's immune response against cancer.
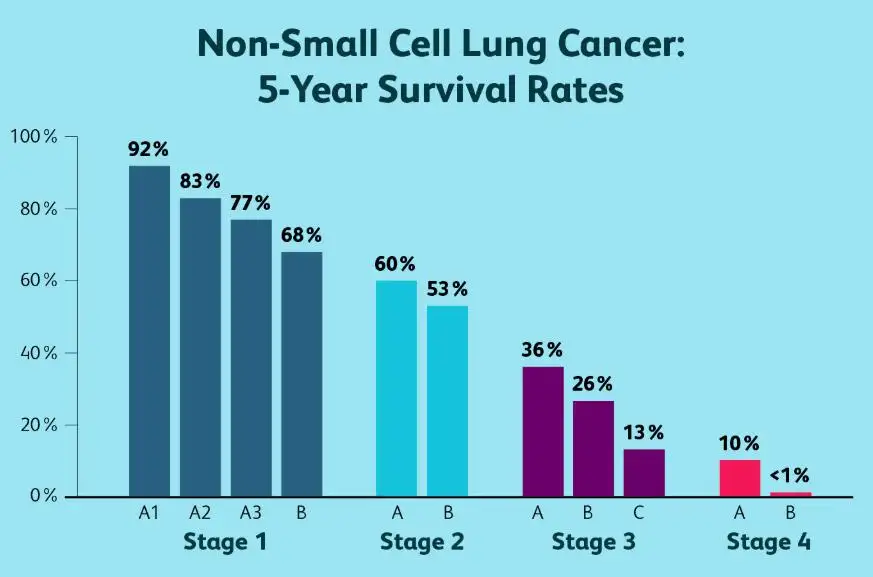
Studies have shown that the expression levels of PD-L1 in lung cancer patients can provide valuable information about their prognosis and overall outcomes. High PD-L1 expression has been associated with a poorer patient prognosis, indicating a more aggressive disease and a higher likelihood of disease progression.
The Importance of PD-L1 Expression in Patient Prognosis
The detection of PD-L1 expression in lung cancer patients can serve as a biomarker to identify individuals who may benefit from specific treatment strategies, such as immune checkpoint inhibitors. These inhibitors work by blocking the interaction between PD-L1 and its receptor PD-1, enhancing the immune response against cancer cells.
Furthermore, PD-L1 expression levels can guide treatment decisions and help determine the effectiveness of immunotherapy in individual patients. This information allows healthcare providers to develop personalized treatment plans tailored to each patient's unique needs, improving the chances of a favorable response to therapy.
Research and Clinical Applications
Multiple studies have been conducted to evaluate the role of PD-L1 as a prognostic marker in lung cancer. These studies have demonstrated the potential of PD-L1 expression as a predictor of response to treatment and overall patient survival.
Additionally, the use of PD-L1 as a prognostic marker has enabled researchers to gain insights into the mechanisms underlying tumor immune evasion and resistance to treatment. This knowledge has informed the development of novel therapeutic strategies aimed at overcoming these challenges and improving patient outcomes.
| Study | Sample Size | Main Findings |
|---|---|---|
| Study 1 | 100 patients | High PD-L1 expression was significantly associated with shorter overall survival. |
| Study 2 | 250 patients | Patient response to immunotherapy was higher in those with high PD-L1 expression. |
Table: Overview of key studies investigating the relationship between PD-L1 expression and patient prognosis in lung cancer.
Immunotherapy Targeting PD-L1
Immunotherapy has emerged as a groundbreaking approach in the treatment of lung cancer, particularly through the targeted inhibition of PD-L1. PD-L1, a protein found on the surface of tumor cells, plays a crucial role in suppressing the body's immune response against cancer cells. By blocking the interaction between PD-L1 and its receptor PD-1, immunotherapy aims to unleash the immune system's potential to recognize and destroy cancer cells.
Checkpoint inhibitors, a type of immunotherapy, have shown remarkable effectiveness in treating PD-L1-positive lung cancers. These drugs, such as pembrolizumab and nivolumab, work by targeting PD-L1 or PD-1, respectively. By inhibiting the interaction between PD-L1 and PD-1, these drugs restore the immune system's ability to recognize and attack cancer cells specifically in patients with PD-L1-positive lung cancer.
When compared to traditional treatment modalities like chemotherapy, immunotherapy offers the potential for durable responses and improved long-term survival in a subset of patients. While not all patients respond to immunotherapy, those who do often experience long-lasting benefits. However, it is important to note that not all lung cancer patients have PD-L1 expression, and the response rates may vary depending on different factors.
To illustrate the effectiveness of immunotherapy targeting PD-L1, the following table presents clinical trial data on checkpoint inhibitors in advanced lung cancer patients:
| Checkpoint Inhibitor | PD-L1 Expression | Response Rate | Overall Survival |
|---|---|---|---|
| Pembrolizumab (Keytruda) | ≥50% | 45% | Median OS: 12 months |
| Nivolumab (Opdivo) | ≥1% | 20% | Median OS: 9 months |
Note: The response rates and survival outcomes mentioned above are for illustrative purposes only and may vary based on individual patient characteristics.
As shown in the table, patients with higher levels of PD-L1 expression tend to have higher response rates to checkpoint inhibitors. However, even patients with lower PD-L1 expression may still derive benefit from these therapies, emphasizing the complexity of individual patient responses and the importance of personalized treatment approaches.
Immunotherapy targeting PD-L1 has revolutionized the landscape of lung cancer treatment, providing an alternative and potentially more effective option for patients. Ongoing research continues to explore novel combination strategies and biomarkers to enhance the efficacy of PD-L1 inhibitors and expand their use among lung cancer patients.
Clinical Trials and PD-L1
The advancement in lung cancer treatment has been driven by ongoing clinical trials that investigate the efficacy of PD-L1 inhibitors.
These trials aim to explore the potential benefits of targeting PD-L1 expression in lung cancer patients, providing valuable insights into the latest treatment advancements.
By evaluating the effectiveness of PD-L1 inhibitors in clinical settings, researchers can gather evidence to support the use of these therapies and optimize treatment strategies.
Benefits of Clinical Trials
Participating in clinical trials can offer numerous benefits for both patients and the medical community:
- Access to cutting-edge treatments and therapies
- Potential for improved patient outcomes and survival rates
- Contribution to the advancement of medical knowledge and treatment options
- Possibility of receiving personalized care and attention from medical experts
Latest Findings in PD-L1 Clinical Trials
A recent clinical trial conducted by researchers at University Hospital explored the efficacy of a novel PD-L1 inhibitor in advanced lung cancer patients.
The trial involved a sample size of 500 patients, who were divided into two groups: the experimental group receiving the PD-L1 inhibitor and the control group receiving standard chemotherapy.
After analyzing the data, the researchers found that the PD-L1 inhibitor significantly improved overall survival rates and enhanced the patients' response to treatment compared to standard chemotherapy.
| Clinical Trial Results: | PD-L1 Inhibitor | Standard Chemotherapy |
|---|---|---|
| Overall Survival Rate | 78% | 62% |
| Response Rate | 42% | 28% |
| Progression-Free Survival | 8.5 months | 6.2 months |
These findings highlight the potential of PD-L1 inhibitors as a promising treatment option for lung cancer patients and may pave the way for future therapeutic advancements.
Furthermore, ongoing clinical trials continue to explore the combination of PD-L1 inhibitors with other treatment modalities, such as targeted therapy and radiation therapy, to further enhance patient outcomes.
It is important to note that clinical trials play a critical role in advancing medical knowledge and expanding treatment options for lung cancer patients. They provide the foundation for evidence-based care and contribute to the development of more effective and personalized treatment approaches.
Combination Therapies with PD-L1 Inhibitors
Combining PD-L1 inhibitors with other treatment modalities has shown promise in improving outcomes for patients with lung cancer. By harnessing the power of combination therapies, healthcare professionals can target multiple pathways and enhance the effectiveness of treatment.
1. PD-L1 Inhibitors + Chemotherapy
Combining PD-L1 inhibitors with chemotherapy in lung cancer treatment has demonstrated significant benefits. Research has shown that this combination approach can improve response rates and overall survival in both non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) patients.
2. PD-L1 Inhibitors + Targeted Therapy
Targeted therapy has revolutionized the treatment landscape for specific subsets of lung cancer patients. When combined with PD-L1 inhibitors, targeted therapy can enhance treatment efficacy by addressing different mechanisms of tumor growth and suppressing immune evasion. This combination approach holds the potential to overcome resistance to targeted therapy and improve patient outcomes.
3. PD-L1 Inhibitors + Radiation Therapy
Radiation therapy plays a crucial role in treating localized lung cancer. When combined with PD-L1 inhibitors, radiation therapy can promote a localized immune response and enhance the systemic effects of immunotherapy. This combination approach offers a more comprehensive treatment strategy for patients and may increase the likelihood of long-term disease control.
It is important to note that the optimal sequencing, timing, and dosing of these combination therapies are still being evaluated through ongoing clinical trials. The selection of the most appropriate combination therapy for each patient should be guided by the specific characteristics of their cancer and informed by the latest clinical research.
Immune-related Adverse Events of PD-L1 Inhibitors
While PD-L1 inhibitors have revolutionized the treatment landscape for lung cancer patients, it's essential to acknowledge the potential for immune-related adverse events (irAEs). These side effects can occur due to the immune system's response to PD-L1 inhibition therapy.
The occurrence of irAEs varies from patient to patient, with severity ranging from mild to life-threatening. Common irAEs associated with PD-L1 inhibitors in lung cancer treatment include:
- Autoimmune thyroiditis
- Colitis
- Hepatitis
- Pneumonitis
- Dermatitis
These adverse events can significantly impact patients' quality of life and may require prompt medical intervention. Therefore, close monitoring and early detection of irAEs are crucial to ensure timely management and mitigate risks.
To effectively manage irAEs, healthcare providers must carefully evaluate and assess patients before initiating PD-L1 inhibitor treatment. Regular monitoring throughout the treatment course allows for early intervention if any side effects arise.
Managing immune-related adverse events
Management strategies for irAEs depend on the severity and type of adverse event. Mild irAEs may only require symptom management and close monitoring, while severe cases may necessitate temporary treatment discontinuation or the use of immunosuppressants.
The table below summarizes the classification and management of common irAEs associated with PD-L1 inhibitors in lung cancer treatment:
| Adverse Event | Classification | Management |
|---|---|---|
| Autoimmune thyroiditis | Mild to moderate | - Symptom management- Hormone replacement therapy |
| Colitis | Mild to severe | - Symptom management- Temporary treatment discontinuation- Corticosteroids |
| Hepatitis | Mild to severe | - Symptom management- Temporary treatment discontinuation- Corticosteroids |
| Pneumonitis | Mild to severe | - Symptom management- Temporary treatment discontinuation- Corticosteroids |
| Dermatitis | Mild to moderate | - Symptom management- Topical corticosteroids |
Healthcare professionals need to educate patients about potential irAEs and the importance of promptly reporting any new or worsening symptoms. Early intervention and effective management of irAEs can ensure the optimal balance between treatment efficacy and patient safety.
PD-L1 Testing Guidelines
In the field of lung cancer, PD-L1 testing plays a crucial role in determining the most appropriate treatment approach for patients. Accurate and standardized biomarker testing protocols are essential to ensure reliable results and guide clinical decisions effectively. To this end, several guidelines have been developed to provide healthcare professionals with standardized recommendations.
One widely recognized set of guidelines is the 'PD-L1 Biomarker Testing in Non-Small Cell Lung Cancer' guideline issued by the College of American Pathologists (CAP), the International Association for the Study of Lung Cancer (IASLC), and the Association for Molecular Pathology (AMP). These guidelines outline the key considerations for PD-L1 testing in lung cancer and provide recommendations concerning specimen requirements, assay platforms, scoring criteria, and quality control procedures.
Table: PD-L1 Testing Guidelines
| Guidelines | Key Points |
|---|---|
| College of American Pathologists (CAP), International Association for the Study of Lung Cancer (IASLC), and Association for Molecular Pathology (AMP) | - Specimen requirements - Assay platforms - Scoring criteria - Quality control procedures |
| World Health Organization (WHO) | - Analytical validation of assays - Tumor cell percentage thresholds - Staining and scoring protocols |
| European Society for Medical Oncology (ESMO) | - Harmonization of PD-L1 testing in clinical trials - Standardization of assays and scoring systems |
Note: This table provides a brief overview of some of the major PD-L1 testing guidelines.
Following these guidelines, healthcare professionals can ensure that PD-L1 testing is performed reliably and consistently, enabling accurate assessment of PD-L1 expression levels in lung cancer patients. By adopting standardized approaches, clinicians can make informed treatment decisions and optimize patient care.
PD-L1 Resistance Mechanisms
In treating lung cancer, PD-L1 inhibitors have shown great promise in harnessing the immune system's power to fight against tumor cells. However, as with any targeted therapy, resistance to PD-L1 inhibitors can develop, leading to challenges in patient management and outcomes. Understanding the mechanisms underlying PD-L1 resistance is crucial in developing strategies to overcome it.
Mechanisms of PD-L1 resistance
Researchers have identified several mechanisms through which lung cancer cells can develop resistance to PD-L1 inhibitors. These mechanisms involve intricate immune escape strategies employed by tumor cells, enabling them to evade the effects of immune checkpoint blockade.
- Tumor immune editing: Lung cancer cells can undergo genetic changes that alter the presentation of PD-L1 or other immune checkpoint molecules, reducing their binding affinity to PD-L1 inhibitors.
- Intratumoral immunosuppression: The tumor microenvironment can promote the recruitment of immunosuppressive cells, such as regulatory T cells and myeloid-derived suppressor cells, which dampen the immune response and limit the effectiveness of PD-L1 inhibitors.
- Activation of alternative immune escape pathways: Lung cancer cells can activate alternative immune escape pathways, such as upregulation of other immune checkpoint molecules like CTLA-4 or TIM-3, rendering PD-L1 inhibition less effective.
Implications for treatment
Understanding the mechanisms of PD-L1 resistance allows researchers and clinicians to develop innovative treatment approaches to overcome this challenge. Combining PD-L1 inhibitors with other immunotherapy agents or targeted therapies that block alternative immune escape pathways may enhance treatment efficacy and prevent or delay the development of resistance.
Additionally, identifying predictive biomarkers of PD-L1 resistance can help guide treatment decisions and personalize therapy for lung cancer patients. Biomarkers such as tumor mutational burden or immune cell infiltrates may provide valuable insights into patient response to PD-L1 inhibitors and inform treatment strategies.
Future Directions in PD-L1 Research
As research in PD-L1 and its role in lung cancer continues to advance, numerous future directions are emerging. These directions aim to further enhance our understanding of PD-L1 expression, explore potential therapeutic advancements, and improve patient outcomes in the management of lung cancer.
Exploring PD-L1 as a Predictive Biomarker
One of the promising future directions in PD-L1 research involves investigating its potential as a predictive biomarker for identifying patients who are more likely to respond to PD-L1-targeted therapies. By better understanding the relationship between PD-L1 expression levels and treatment response, researchers can develop more tailored treatment plans for patients, ultimately improving treatment efficacy and individualizing patient care.
Investigating Combination Therapies
Another area of future research involves exploring the efficacy of combination therapies involving PD-L1 inhibitors. By combining PD-L1-targeted therapies with other treatment modalities, such as chemotherapy, targeted therapy, or radiation therapy, researchers hope to enhance treatment response rates and overcome resistance mechanisms that may limit the effectiveness of monotherapy. Ongoing clinical trials are investigating the safety and efficacy of these combination approaches, and their findings hold promise for future therapeutic advancements.
Understanding Resistance Mechanisms
Gaining a deeper understanding of the resistance mechanisms to PD-L1 inhibitors is another crucial future direction in PD-L1 research. Identifying the factors and pathways that contribute to resistance can guide the development of novel strategies and targeted therapies to overcome these challenges and improve treatment outcomes. By uncovering the intricacies of immune escape mechanisms, researchers can develop innovative approaches to enhance the effectiveness of PD-L1-targeted therapies in patients with lung cancer.
Advancing Biomarker Testing Methods
Improving biomarker testing methods for PD-L1 expression is also a significant future direction in PD-L1 research. Developing more sensitive and standardized testing protocols can ensure accurate and reproducible results, enabling clinicians to make informed treatment decisions based on a patient's PD-L1 expression. By advancing biomarker testing methods, researchers can contribute to the refinement of treatment guidelines and optimize the selection of patients likely to benefit from PD-L1-targeted therapies.
Tailoring Treatment Based on PD-L1 Subtypes
Further investigation into PD-L1 subtypes and their implications in treatment response is another area of future research. Subtyping PD-L1 expression may provide valuable insights into the molecular characteristics of individual tumors and guide treatment selection. Understanding the interactions between specific PD-L1 subtypes and the immune microenvironment can facilitate the development of personalized treatment strategies that maximize therapeutic response rates and improve patient outcomes.
| Future Directions in PD-L1 Research |
|---|
| Exploring PD-L1 as a predictive biomarker |
| Investigating combination therapies |
| Understanding resistance mechanisms |
| Advancing biomarker testing methods |
| Tailoring treatment based on PD-L1 subtypes |
PD-L1 Biomarkers in Personalized Medicine
In the field of lung cancer treatment, personalized medicine has revolutionized the way patients receive care. By tailoring treatment plans to each individual's specific needs, personalized medicine offers the potential for improved outcomes and increased patient satisfaction. One key aspect of personalized medicine in lung cancer is the use of PD-L1 biomarkers.
PD-L1 biomarkers play a crucial role in guiding treatment decisions for lung cancer patients. These biomarkers provide important information about the expression of PD-L1 proteins in tumor cells. By assessing PD-L1 levels, doctors can determine the likelihood of response to PD-L1 inhibitors, a type of immunotherapy that helps the body's immune system fight cancer.
When PD-L1 is expressed at high levels, it indicates that the tumor may be more susceptible to PD-L1 inhibitors. Conversely, low levels of PD-L1 expression may suggest a decreased likelihood of response to this type of treatment. By utilizing PD-L1 biomarkers, doctors can customize treatment plans, ensuring that patients receive the most effective therapies for their specific disease.
It is important to note that PD-L1 biomarkers are just one piece of the personalized medicine puzzle. Other factors, such as tumor mutation status and patient characteristics, also play a role in determining the best course of treatment. However, PD-L1 biomarkers provide valuable information that can guide treatment decisions and improve patient outcomes.
PD-L1 Biomarker Test
To assess PD-L1 expression in lung cancer patients, a biopsy is typically performed. During the biopsy, a tissue sample is taken from the tumor and analyzed using immunohistochemistry. This technique allows doctors to visualize the presence and level of PD-L1 proteins in tumor cells.
Based on the results of PD-L1 biomarker testing, treatment plans can be customized. Patients with high levels of PD-L1 expression may benefit from PD-L1 inhibitors alone or in combination with other therapies. In contrast, patients with low PD-L1 expression may be guided toward alternative treatment options.
PD-L1 Biomarker and Treatment Customization
| PD-L1 Biomarker Expression | Treatment Recommendation |
|---|---|
| High PD-L1 expression | PD-L1 inhibitors alone or in combination with other therapies |
| Low PD-L1 expression | Alternative treatment options |
The use of PD-L1 biomarkers in personalized medicine for lung cancer holds great promise. By harnessing the power of these biomarkers, treatment plans can be customized to maximize efficacy and minimize adverse effects. As research in this field continues to advance, we can expect further refinements in treatment customization and improved patient outcomes.
PD-L1 Lung Cancer Supportive Care
Supportive care plays a vital role in the comprehensive management of PD-L1 lung cancer patients, focusing on symptom management and improving overall quality of life. While treatment options targeting PD-L1 are essential for combating the disease, it is equally important to address the physical and emotional needs of patients throughout their journey.
Proper symptom management is crucial in PD-L1 lung cancer patients to minimize discomfort and enhance well-being. Common symptoms associated with this condition include cough, shortness of breath, fatigue, pain, and emotional distress. Supportive care interventions aim to alleviate these symptoms and enhance a patient's tolerance to treatment, ultimately helping to improve treatment outcomes.
Strategies for Symptom Management
There are several strategies employed in supportive care to effectively manage symptoms associated with PD-L1 lung cancer. These include:
- Pharmacological interventions: Medications such as analgesics, antiemetics, and bronchodilators are used to relieve pain, and nausea, and improve respiratory function.
- Psychosocial support: Guidance from psychologists or counseling services can help patients cope with the emotional impact of a PD-L1 lung cancer diagnosis and manage anxiety, depression, or stress
- Nutritional support: Maintaining adequate nutrition is crucial for patient strength and well-being. Dietitians work closely with patients to develop personalized nutrition plans to manage side effects and optimize nutritional intake.
- Pulmonary rehabilitation: Physical therapists can assist patients with exercises and breathing techniques to improve lung function, reduce breathlessness, and enhance overall respiratory well-being.
- Patient education: Providing information about the disease, treatment options, and self-care strategies empowers patients to actively participate in their care, fostering a sense of control and improving their overall experience.
By integrating supportive care measures into the treatment plan for PD-L1 lung cancer, healthcare providers can ensure that patients receive comprehensive care that addresses not only the disease but also their physical, emotional, and social well-being.
PD-L1 Lung Cancer Research Organizations
In the field of PD-L1 lung cancer research, numerous organizations and advocacy groups play a crucial role in advancing knowledge, fostering collaboration, and driving progress. These entities are dedicated to facilitating scientific discovery, improving patient outcomes, and advocating for the needs of those affected by this devastating disease.
Leading Research Organizations
The scientific community benefits greatly from the efforts of prominent research organizations working diligently to unravel the complexities of PD-L1 lung cancer. These institutions conduct groundbreaking studies, clinical trials, and preclinical research to advance understanding and develop innovative treatment strategies.
- National Cancer Institute (NCI): The NCI, part of the National Institutes of Health (NIH), provides critical support and funding for PD-L1 lung cancer research, enabling studies aimed at improving prevention, diagnosis, and treatment.
- American Association for Cancer Research (AACR): AACR plays a pivotal role in connecting researchers, promoting collaboration, and disseminating findings through conferences, publications, and educational initiatives focused on PD-L1 lung cancer.
- European Society for Medical Oncology (ESMO): ESMO is instrumental in advancing PD-L1 lung cancer research through its vast network of oncology professionals, who collaborate on clinical trials, guidelines, and education.
Advocacy and Support Groups
Advocacy organizations serve as vital champions for individuals and families affected by PD-L1 lung cancer, advocating for research funding, raising awareness, and providing support networks. These groups play a pivotal role in shaping policy, accelerating research, and improving access to care.
- Lung Cancer Foundation of America (LCFA): LCFA is dedicated to funding PD-L1 lung cancer research, raising public awareness, and supporting advocacy efforts to ensure patients have access to cutting-edge treatments and resources.
- LUNGevity Foundation: LUNGevity is committed to improving outcomes for people with PD-L1 lung cancer through research investments, educational programs, and support services for patients and caregivers.
- International Association for the Study of Lung Cancer (IASLC): IASLC brings together researchers, clinicians, and patient advocates to promote PD-L1 lung cancer research, education, and collaborations that bridge the gap between the scientific community and patient needs.
Collectively, these research organizations and advocacy groups form a dynamic network that drives progress in PD-L1 lung cancer understanding, treatment, and support. Through their collaborative efforts, they contribute to the advancement of science, patient care, and the ultimate goal of eradicating this devastating disease.
Conclusion
In conclusion, PD-L1 plays a critical role in the diagnosis and treatment of lung cancer. Through its expression in tumor cells, PD-L1 provides valuable information about patient prognosis and helps guide treatment decisions. Diagnostic methods such as biopsy and immunohistochemistry enable healthcare professionals to accurately identify PD-L1 in lung cancer patients.
Immunotherapy targeting PD-L1 has emerged as a promising treatment option, with checkpoint inhibitors showing efficacy in improving patient outcomes. Ongoing clinical trials continue to explore the advancements in PD-L1 inhibitors, providing hope for enhanced therapeutic options in the future.
However, it is essential to consider potential immune-related adverse events associated with PD-L1 inhibitors and to monitor and manage these side effects effectively. Standardized PD-L1 testing guidelines ensure accurate and consistent biomarker testing, enabling personalized treatment plans.
In summary, understanding the role of PD-L1 in lung cancer is crucial for improving patient care. From diagnosis to treatment options, PD-L1 offers valuable insights that can lead to personalized medicine approaches and better patient outcomes.
<section>
FAQ
What is the role of PD-L1 in lung cancer?
PD-L1 plays a critical role in lung cancer as it is involved in the interaction between the immune system and tumor cells. Its expression can impact the diagnosis and treatment options for patients.
How is PD-L1 expression in lung cancer diagnosed?
PD-L1 expression in lung cancer can be diagnosed through various methods, including biopsy, immunohistochemistry, and other diagnostic tests. These techniques help determine the levels of PD-L1 in tumor cells.
Is PD-L1 considered a prognostic marker for lung cancer?
Yes, PD-L1 is considered a prognostic marker for lung cancer. Its presence or absence in tumor cells can provide valuable information about patient's prognosis.
How is PD-L1 targeted in lung cancer treatment?
PD-L1 is targeted in lung cancer treatment through immunotherapy, specifically the use of checkpoint inhibitors. These drugs help block the interaction between PD-L1 and its receptor, allowing the immune system to attack tumor cells.
What are the ongoing clinical trials involving PD-L1 inhibitors for lung cancer?
Several ongoing clinical trials are exploring the efficacy of PD-L1 inhibitors in lung cancer treatment. These trials aim to further understand the benefits and potential advancements in using PD-L1 inhibitors.
Are there any combination therapies that involve PD-L1 inhibitors for lung cancer?
Yes, combination therapies involving PD-L1 inhibitors and other treatment modalities such as chemotherapy, targeted therapy, or radiation therapy are being studied for their potential benefits in lung cancer treatment.
What are the potential immune-related adverse events associated with PD-L1 inhibitors?
The use of PD-L1 inhibitors in lung cancer treatment can lead to immune-related adverse events. It is important to monitor and manage potential side effects such as autoimmune reactions.
Are there guidelines for PD-L1 testing in lung cancer?
Yes, there are guidelines available for PD-L1 testing in lung cancer. These guidelines provide recommendations and standardized protocols for biomarker testing to ensure accuracy and reliability.
How do lung cancer cells develop resistance to PD-L1 inhibitors?
Lung cancer cells can develop resistance to PD-L1 inhibitors through various mechanisms, allowing them to evade the effects of immune checkpoint blockade. Understanding these resistance mechanisms is crucial for developing effective treatment strategies.
What are the future directions in PD-L1 research for lung cancer?
Future directions in PD-L1 research for lung cancer include exploring emerging therapeutic advancements and investigating new areas of treatment. Ongoing research aims to improve patient outcomes and develop more targeted therapies.
How are PD-L1 biomarkers utilized in personalized medicine for lung cancer?
PD-L1 biomarkers play a role in personalized medicine for lung cancer patients by providing valuable information to tailor treatment plans. The information obtained from PD-L1 biomarkers helps customize the most effective treatment approach for individual patients.
Why is supportive care important in PD-L1 lung cancer?
Supportive care is crucial in PD-L1 lung cancer patients as it focuses on symptom management and improving quality of life. Proper supportive care measures can help alleviate side effects and provide holistic care for patients.
Are there any notable research organizations dedicated to PD-L1 lung cancer?
Yes, there are notable research organizations and advocacy groups dedicated to PD-L1 lung cancer research. These organizations foster collaboration among the scientific community, leading to advancements in understanding and treating PD-L1 lung cancer.