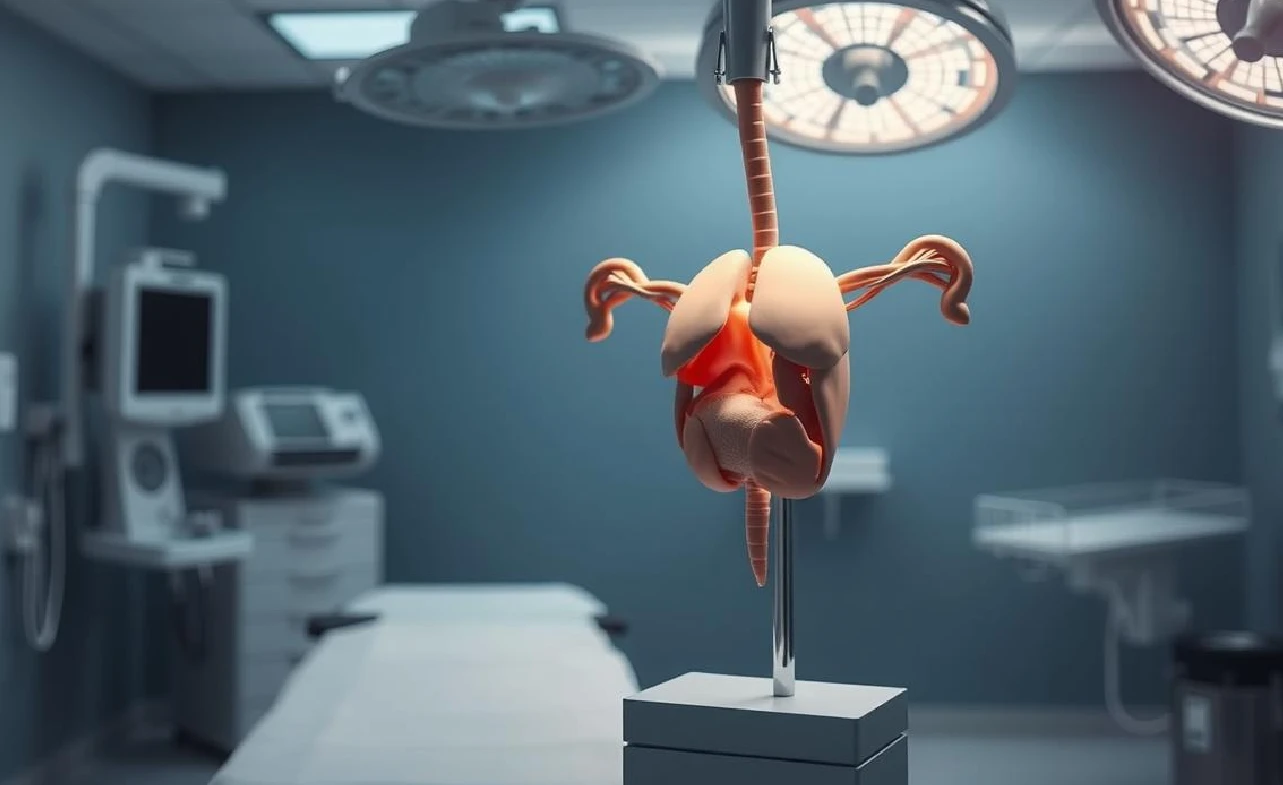
Prostate Cancer Treatment – There are many ways to treat prostate cancer, including orchiectomy, or surgical castration. This method involves removing the testicles to lower hormone levels. It can slow down prostate cancer cell growth.
Orchiectomy reduces testosterone levels, which helps stop cancer growth. It’s a hormone therapy that aims to lower male hormones. This makes orchiectomy a key part of treating prostate cancer, offering a unique way to manage the disease.
Understanding the Role of Testosterone in Prostate Cancer
Testosterone is key in prostate cancer growth. It makes cancer cells grow faster. This is why it’s a big part of treatment plans.
cNRuVTOfJaAlvpkcVnUZoLTafNCTV+xp6lqEU8cNraxGGxtxiKMnkk9WY+p/SswnmkJpM0C0irIcBmpBHmliXNWlj4oHGFyqYuKiePFaG0VFJHxRYt0rGXIMVA1XZ0xVF+tIytZjGqI1IajagBhphp5phoGJRRSigGKBTwtCipQtFiGyPbSFalxSEU7E8xXZagYVbZagcUWGmVWqM1K4qButIpMQ00mgmmmgYtJRSZpiuLmkzSZpKAOpp2aZS17R+TDs1FMm5akoIyKQ0Zbjaas2s2CBSTx4JNVQSjUjXc3UfIp+aoW0+RgmrgORTIaJAaXNMzS5oEPzS5pmaXNAx2aWmZozQA+im5ozQA+im5ozQA6muflozTZPu0FR3My6bg1mP96tG671mt1pHqUdgFOFMpwoNyRakFRLUgNA0SLUgqIVItItEopwpgp4pGsUSJ1q5H0qmtXYulCMMSvdKt4tU4zh60bxMjNZo+V6Dy7mxatlasGqNo/SrxpmMmxjUw1I1RmmK42ig0lIYhGahdKnoIzQNMpEYpyPipXjqErg0F3uWkfNTA1SjOKtIc4oIZOKeKYKkFBI4UtJS0ABphpxppoAYRUTCpjUZFIpELCoyKnNRNSKRSv7ZbvT7i2cZWSNhg+uOD+deMmvcNuWA9TivEp12zyL0wxH61xYpapnoYN6NEdFFFch2hRRRQAUUUUAFFFFABRRRQAUUUUAFFFFABRRS0AFFLilApDEApcUuKXFA1EbijFP20u2grkI8UYqXbRtoHyEeKUCn7acFoKUBgWnqlSKlSpHmg2hSuRqlTpFmpkhqzHDQehRwrZXSD2qQQe1bGn6Tc6hcLb2kEk8zdI4kLMfwFd9pfwf1a5VX1C4t9PQ9Vc+Y/5Dj9adjrlTo0l77seV/Z/akNv7V7gPg1poXDeIJS3+zbrj+dZOp/B68ijLaXqdvdkf8s5EMTH6Hkfyp2IU8PLS/wCB5CYPao2hwCcV0Oo6Pd6Xdva31tJbzr1SRcH6j1HuKTSNPF7rVnblcq0q7h/sjk/oDU21NJ4WPLdHoeg6d/ZmhWVptw6Rhn/3m5P6n9K0cU48kk96RiWYk9TXUtNDznQCjNIabmquQ6Vh4NLmo80uaZm42HZoJpM0maQrC1HPNHbwPNK4SKMZZj/nrTt3PHJ7CuE8W62by4Gn2z7oYzglf42/zxUTlZHZhaHO+aWyMfW9Wk1a+aU8IOET0HavQtItPsOkWlsRhkjG7/ePJ/U1z/h7ws0Lpeagg3jmOE9j6t/h+fpXXVEFbVmmIqqbshKKWkrQ50FKKSnCkaQ3HgZrqvCmkWjrLq1zAkktsdsDMOVbHJH5iuXQV29iwtvBUBXrKzsfzI/pUPsdGIlL2ahF7uxxHi3WXDyDcSRkDPrXnkjliSTkmtrxFO0l+4J71hMal6aH1eGpqhQUUNZqbuprGkzUkOepKHqaOQg5zVUVIp5oRrSm7npHgfW2S5RHb5lIwa6jxZZJDqK3MY+S5Xf+Pf8ApXmHhiYx6mnvXreuH7R4ZspiMujhc+xB/wABVPe54OY01SxkZx+1ozj2FMqRqjqkc1ZWYUUmaM0GItJQTSUFRVxa8+8RrJpnij7ZAcOds4+p6/yNegjrUFx4Im8SXccyusFvEm2WaQcDknA9TzUSVzqgoQTc3ZBaXMV7ZxXUJ/dyqGHt6j8DxUpx2NbVlN4Z8J2C2EIFzsYnfOA5yeuOMAVdt/EWg6gfLmsrYr3OwKR+NXqtyOaolzKm2jlTUcsscMTSyuscaDLO3QCtjxHBpOm2TajaXu6HcF8g8vk9lPf8a4ELP4nvC0paPTIm4ReN59M9z6nt2qW+xpBKpHmWiCVpvE04ALw6XG30aUj/AD+H1rchgit4ViiQJGowqjoKesSQxrHGgRFG1VA4ApaEiZjTTTTjTTQQFNpc03NAwpKWm0DuLQOtJQDzQFy5CKtdqpwtzVoHIpo66TQUh6UtNYgCmdDtYo3IrOfrV+5as9+TUs4ZvUjNRtUpFMK0ibkRphqUrTCtAXGU5aTFKtANkyCpKjSpKpGTYGmmlNJTFca1QSCpzUElIEVZKrP1qzJVV+tI0TGGmk0pptAxaaaWkoAKTNBNITQB1Ipwpgpwr2j8nFpaMGjFA7DJE3LWfNGQa0qgmj3DIqWXFlKKQo1akE24VkyKVNSQTFSOaCmrm0DRmoI5Qw61JmmRYkzS5qPNLmgCTNGajzS5oAfmlzUeaN1AEmaXNRbwO9RPcqvekNK5ayB1qOSVQvWs6W+x3qpJfZ70XNoUyxcyAk1QY801py9N3UHo01ZD6UU0U4UGo8VIpqIGng0FImWpFqFTUqmkWiVaeKYtPFSbxRInWr0Q4FVIl5q9GtNHHi52Vhs6ZSsmZdrVuMuVrMuosE0zyFIZavgitVG3IKwkbY9attLkUIUkWGqM080w0yUNop1JikMTFGKWigBMZqJ0qegrkUDTKwXmp0pCMUoOKBtk4p4qNTxTwaCSQUtMzS5oAWmmlJppNACGmGnE00mgaGNUTVITUbUikMBwwPvXjGo7f7RuShyplcg+2TXrGtXDWui3s6HDpC20+hPH9a8eJrhxT2R6GDWjY2iiiuQ7gooooAKKKKACiiigAooooAKKKKACiiloAKWgCnAUDSEApwFKBTwtI0jG40LTwlSKlTLHQdEaVyAR07y6tLFUgh9qDpjhmyl5VHlVf8j2o8j2oNFhWURFThFV3yPaniD2oLjhWVFiqxHDVlLf2rR07SbrUbuO1sreSeeQ4WONck/59aDrp4VR1ZRig9q9J8G/DC41ZUv9ZMllp/VVIxLMPYH7o9z+HrXXeEfhta+HVTUdcaKe/GGjtxykJ9T/AHm/Qe/Wt/VtdRFID5NWkZyrym/Z4f7/APInhfSfDll9l0q0itowOdg+ZvcnqT9awr/xKq5LSYH1rlNa8S7SVVsn61yFzqMty5LsSPSrSR6eEyuEVzVdzv5PF8KtxKT9Ks2fjJGcDzvwJry7zSaeshBourno/UcNNWse4tBpXi/TvseowrICPkkHDxn1U/5FefaR4H1DSPG11aPC0qW0DSRTKMCRW4Uj36gjsQam8FatLDdiNmJX3Nesag4fRkvUwJY/l3f7J6j+VTJcrPncZTqYGt7OD92R5xKhicowIPoRUda2rarFCkRmTzGYfNgDOB0rOX7LeYe1uEGeqsDwf5/zqlO5rGjNw5miJULtgf5FRHrVu5V1CAxbUAwGHR/eqpqk+phOFtBKXNNzRmrucNSNmOzSE0mfmA7msPXPEsWmRGK2ZZLlgQWxwv0/xpSkkbYfCyqu+y7kXifXBYQtZwN/pUgw5H/LMHt9aqeFNEEarqVyuZG5hU/wj+99fSsPQ7F9b1fdOS0anzJmPf2/GvRlUKAAAABgAdqziuZ8zOjEVIwj7KGw+ikorQ4AopaSgpAKcKbSg0jSG5KDiuytm8zwbbDp5bOp/M1wGoalb6bbebO43EfJGD8zf4D3rL0r4gTxahP9qLvazjHlJ0QjgYFZyPQ+rTqxTXR3KOuKRqEmfWshq6HVMX+bqKN1AOCGHNYbpzSkup9TBc1JLsVGFNxU7JTdlSczi7jQKkUUBKlRCSBQa04O5s+G1xqKPjOK9b1JkHhmO3WRWlBVioPIGDziuB8KaPIzh2GO5PpXM6xrF/a6vK8c0kc6yHJU9Oe1U7HmY2ksTW0fwHauajzXJWvjVywGoReZ/wBNYwA34jof0rctta066UGK8hyf4XbYfyNNNM4cRTktzSoqu15bIMtcwAepmX/GqkmvaTH9/UbYfRi38gad0cvJLsaVGaxW8U6Ov/L6D/uxv/hUTeLtIH3ZJ3PtDj+ZpXR0Uqcr7HXaPYHU9SitwcJ96Rv7qjrUvjbxClmgtLXCRou2NB2HrXNab8RbbSVnMGnyzSTKF3u4XaPYDNYt9q0Ovyz3BhaKdRuILbhj2oTSdzrw+FcsTz1V7q29TPnu5ZXLM5yaYlzLG2Vciompveocnc9tztobFtefbbi3jvf3kMbcJ0B574616Z4hsLM6fZalYQpFDKux0QYCtj07d/yryO2YrKpHY165p8jT/D+feM7JUK57c4qltc8nM4crp1I97fecu4qI1PJUDdaDjq6MaaYacaaaZkIabSmm0hi0lGaaTTAWjNNJpCaQEySYqdZ/eqG6jeRQaRlY0vPFRyT8VSEhpGcmmdEpe6LK+41ARTutOC07HHKRHspClThaXZTUTJ1CqU9qiZKulKjZKOUFMpMtN6VYdKgYYqbGilcehqTNQA4p4agTHmkpNwpC1MkGNV5DT2eq8j0hoikNVnPNSu1V2PNI0QlJQaSgYUhNGaQ0BcKSlpKBXOpUZq3DAWqCBcmtNSIY9xFevJ2PzbDYf2jGC0yOlRSWxXtSjUBuxmrUcqzL1qOc9CpgEo3RmOhFRGr1zHtzVBjzWidzyakOR2Ks8fcVSYFWzWowyMVTnixSFFjrefHer6OGFYe4o1XrefoKBuJpZozUQbNLuqjMkzRmoy4A5NQSXQXoaVxqLZaLgdTUMl0F6Gs+W896pS3ee9K5rGmaMt771SlvCe9UHnLUzJalc2UEid7hmPWmBixpEjLVdhticcUFXSGxRFqn8g46Vft7TgZFWHthimio1jGKlaBV2W39KqtGVpnVGaY0VIDUfSnA0GqJlNSKahBqVeaRpFk61LGuTUcak1ciTFIc6qiiWJKtoMCoEwKl3gU0ePiKrkyQ1XuI9y1JvzQSCKZyoxZkKtT4Jdp61Yuoxg1nFtjUjXdG1HIGFPrNtpuRWgrZGaZDVh9FFFAgooo4oGFLSZozQA0im1IeRUZFADlbFSBxUHSjdSGWg1Luqrvp4egLE+6mFqjL0wvQFiUvTC9RF6YXoKsSlqaWqIvSFqQ0R3sCXllNbSfclQoSO2R1ryC+sp9Pu5La4QrIhwfQ+49q9gLVzvi+2s5dEluJlAuItohcdTk8r7jGT/k1y4inzK/Y68NU5Xy9zzeig0VwHpBRRRQAUUUUAFFFFABRRRQAUUUUALSikpwoGgAp4FIBUqikaRjcFWpkSlRKsxxUHbSpXGpFVhIfarENvuxxXqnhH4R3F/Gl9r7yWNqcMtuABNIPfP3B+v0ppHfyU6UeaZ5hbWUtxIscMUksh6IilifwFdVYfDPxXfoHj0WaND3nZYv0Yg/pXvFjZ6P4et/I0uygtkA5KjLN9WPJ/GmTa3tP3qqxKrVZfw4/eePj4O+K9ufs9nn+79pGf5VWn+E/jCEZ/skSD/plcRt/WvXn8RMOj/rUDeKCp5f9arlZSeL7L7jxpvh54qU/NoF7+Cg/1qxbfDTxZcMAuh3Ce8rIg/U16y3i8j/lpj8aqz+MOD++/WjkZrGeLe0V+Jzek/B24UrLreowW6dTDbfvHI9NxwB+td1ZRaN4ZtDBpVrHACMPJ1d/q3X8OlcjeeMQAd1yPzrm7/xcXBEZLfXgVSgarA162tZ6duh22reI0VWJkHFcBq/iJ7hmWJjg/wAVYd3qk90T5j5HoKpNITRsepRo0qC93cmknZ2JJyai3UzOaVRzUtmvO2yVTUycmo0XNXLeAyOFAzSWp10o3Oj8JxH7WjY7167qbi28GXLseduB9Sa4PwppxEsY29DXTeN79YNPtNLVv3kh8119FHT8z/KnJ6ngZl+/xkIR7/kcfcTLPDl+e7KOd54wOK5u8LRTtJaFihGTtz8g9/ar6yv5rxqc7hwD69j+Faces2fh4LCqrJMwHnBABn8a5ZScHpqevHnou0FdvoYFn4iubQBRiSP+5Jyv5f1robTUtP1MPsU2sg7M25B+PWuZ1G50y6uvOjikgzy6pjBP45qouqxWbk2kGDjBZzuP4elbxmzXEYWlWjzOPLI7e4tEtebi7hjU9MAsT+GOKpNd6eh4uZJeOiR7f1J/pXEyX0lzNmR2Zie5qOW/VGMatkHhiO9X7RnFHLsNFXqSuamueJhseC1URxnggHJb6muKdnnmLNkkmrt7EDLlGyp+7z1qzommtd6lCm0su7Lew7mo1ZyV23L2cVaKOz8OacNP0qMEfvZfnc/XoPy/nWxTOAOBgelLuroSsrHg1JuUmx9JTHmSNC7uqIOrMcCsu68SaZbZAmeVh2ROPzJFDaW5pToVJ/CjXzSEgVyc/jeBOIrRif8Abk/wFZdz40v5VIhEUPuqZP65qHUXQ2WGa+Jo7x5kjQvI6og6s5wB+Nc7qnjCCAGPTk81+hlkHyj6Dv8Aj+Vce9xfalMGlkmnc9NxJ/IV02l+C5ZQst+5jB/5Zjlv/rVDk3ojppUEtTnJ7q4vp2lnkeSRjyTzV2z0bULj5orWZh67cD8zXoNppNlYqFt7dFI/ixk/nVsj15o5e53QdjZ8M+GRd+DojIR9qUESxEgspycdPUYNcZqugSWsr7Y2wPUV0mn6jc6Zcia2faehB6MPQiunGoaVryqsoW1vD2c/Kx9jT+H0MoYqvhark/ei/wADxWa3dCQVI+oqHYQelewXng/LEhSffGQay5PBilwWQgA84HSl7p6UM2w0tzziG1llYBYya6rQvC8k8ivLHx9K6Z7fw/okYN/eQREEZBbc3/fI5rWk8S6bZWUbaQguZJUDJMy4RQe+OpNO66HNic0m1y0IPXqSzi08M6SPutfSr+6TH3f9oivPrzTbS/bdcxl2/vbiG/MVo3V1NdztNcSNJIxyWY1XJoS7nDS5qScm7yZiSeEtLc5BuF/7aA/zFQt4N05h/r7r/vpf8K6AmijlRMq031OdHgvTR1mum/4Eo/pUg8IaUB/y8n/tr/8AWrepDRyoj2ku5gHwhpR6G5H/AG0B/pSf8IjYA/LPcj8VP9K3jR3o5UbUqjvqR+H/AABpuq3U1vLeXSssRkjC7fmI6jpWDqmlpot5LbwmQo3BL4zx+Fddp99Lp97FdQHEkZyPQ+oP1rd1nRbLxVatf6eAJ8fvYP4lNCirnTSxTo171fgf4M8gYUzFbt7oF3ayFWgcYPXFVodJuZnCrE35Gp5Ge2nCS5k0QWMDS3CKBkk16xcR/wBleDILRjiS5cMR/sjn+eK4l7WLwxYLf3IVpyw8uI/xH/Petm78SReJLe3vIcIscYjaLP8Aq29P/r1W2h5OOk60oKPwp/iUpGqAmldsmmZoOKpK7A000pNNNBmBphpSaaTQMCaaTQTTCaAFzSE0hNNzQMdmmk0maTNAJjxQaQUlI6JfAOFSqKiWplrSKOCbHAUUUVpYwuIRTCKeaYaBpkEi1VkFXX6VUlFZyRrBlYnFG+myVEWqDcn8ymtJUO+mM9FxWJWkqB3prPmm8k0hjWOaiIq0sBNO+zH0oKKNJVt7cjtVZ0IoAZSUtJTFcWkNFIaQHZW3Wpb5ysPBrJju9rDFXkY3C4NenJ6nxWCiorUzdzFq19NZu9RfYPmq9bQiBcmpvc9GpOKgxbzGKy3PNXLqbcTVBm5rWJ81iZJy0FpjruWlzRmrOZGZcLtqGOba2M1buxxWRI+1qhnRBXRuxXQ28mle8AHFYQuSB1pGuSe9FyvZGlLe+9VJLsnvVJpCe9IMk0rlKCRK0xbvTMk09Ii1WY7XPagq6RVWMk9KtRWxJ5FXIrT2q9FbAU7GcplWC09q0obdV7U9EC9qkFOxk5NjlAHSndRTaWmRcjeMGq724ParmaQgGg1jVaM1ramfZ8dq0igpPLFB0xxBQWCpkixVjYBRjFA3iQRMVMDiot2KQvSMJ1XIseZSeZVff70b6Ziyz5lL5tVd9G+gViaVtymsqfgmrxbIqlOOtI0iED4atWF8gVhxthq1Ld+BQgkjQzRmolanZpmY/NJmkzRQMdmjNNpc0gHZo4ptFMAIphp9NNIYylBxTTSZ5oGPLVGWpGaoy1AxxamlqYTRmkMdmkJpuaSgYpNcd46nbFlAPukM59zwP8/WuvzXN+MdPe601LmMZa2JLAf3T1P4ED9awrJuDsb4dpVFc8/ooNFeaeqFFFFABRRRQAUUUUAFFFFABS0lLQAopwpop4pFJDlFTotRoKsxLQddKFyWJKvwRZxUMMfSvWvhH4Pj1G9fXr+INaWbgQIw4km65+i8H6kelNHqLlo0+dnT/D34exaHbQ61rUQbUGAeC3ccW47Eju/8vrXVajqvUBqk1a/xuGa43Ub/ABnmtEgw2HlWl7SpqT3uqkZ+asC81xYwSz9KxdU1jaWUHmuWur55WJJzVxj3PdhSp043kdFd+J3yREfxNZM3iG7cn95j6VitISetMLVpoiJYhL4UaT6vdN1maq730z/ekY/U1TzRmi5m8RIsecx70nmE96hFPAqWHtJMeDmnCkVc1MkZqGbQTYirmpUSpEi9qu21m0zhVHNSd9Kh1ZHBAZGAUc11mi6KzMrFean0bQDlSy816Bp2mW2n2j3l46xQRDczNwAKfwnLjsfChHkhuLYQWug6XJqd8dkMS5x3Y9gPevKtW8R3eq6rNfyNsd2yoU/cXsPwFaHjDxZL4guRFEDFYQn91F6/7R9/5VynU1nKSub5TlrhfEYhe/Lp2Rr20w+0w3MhVYCCXK8kEA5GD3/xqhemG7eOa1Db5BtaALkgjuMdQabANswVJN0zjAQep4wcitDSdC1C511bW3t3R4ZgHkfpGQQeo6n6VzuSTuddSVOi3Nu1kZBs7k28kwgm8tDhm2HA9cnt2/Os569G+IV1qOm3MenbwsE8W6Tag+fn1x9K87kGM46U4ScldnPTrSxFL2rWj2KcrMMkH2NUy5Bq3N901SYHNapnjYmUubQej5cAkDPrXUaPqun6UrM0gkkZdpKg8fTiuRYEUhLU07PQwhXUE1JXud8/jGxBwsczfkP61Xn8aRKv+j2o3Y6yPux+AAriVV2OACT7VftNGu7phhdo9X4Aq+d9RU6ak/cpkl/rd3fSFpZCx7eg+g7Vms0khySa1ZoLCxysl158g6rCOB/wI/0FJZ6lp0dwv2jT98OfmIkO4D+Rqbm04N6VJW8kZsdpLKflU/lXRaX4SuLja84EUfqw5P0FdVpv9mzQiawjhKdmUfMPrnkVohqtQ7nP7SEHaC18ytYaVaacoEEfz93br/8AWrqtJ0yCS0fUNRlaKyjOAF+9K3oKwRzWn4xnaHwfo0UJISSIlseuear0LXNVnCmnbme42fxnpEMnlw6PbtDnAzktj61e+y6frWnSX2kFlkiG6W2Y5IHqK8oYktk13fw2Fx/b8RQnyiGEg7Yx3qb66HoYvA06FJ1KTacfPceRioyanuMea+3G3ccY9M1VY1SOOdSyLltqt9Z/8e11LEPRW4/LpS6jq2pavps1hc3sjRyrgdBgjkHIHqBWeTSg4NFkYc8L81lc8xn8yK4dJMiRWIbPXNejaRKJNC09h1EAB/BjXLeMLNY76C7jGPtGQ/8AvDHP4gitjwxdi40SOP8AigZoz+eR/P8ASs1vY6atTmgmbZNNzSZoFaWOJzuLTgKFXNSqlNIzc7Ee2kK1Y8umtHT5SVUKxFMPFWGSoHGKlo3hIA1T295NazLNbytHIvRkOCKpk4pN1SdKmmrM6iLxfOV231lbXn+0y7W/Mf4USeLNgJtNLtIG/vNlyP5Vy+6gtTJ9lRWyG62G1xXN5KzTEYWTH3fbHp7VxcUl74c1Hc65VhhlBysi12Zaq9zbQ3ULRTIGRhj3HuKhxubKqkuXoSW91FdwJNC+6Nhwf6H3qauQQz+GNQy+6WwlOGI/n7MP1rrI5EliSWJw8bjKsOhFNO5g1qKaaTSmkxTGoiGmk04iozQDjYCaYTQTTSaBATTc0hNIaAFopuaM0BckFBpoNLQdD1gOWp1quDiplNaROCoiSkozRWhgBphpxppoAjfpVSWrTniqkpqJGsCrJVdqnkqE1kdCGGmNUhqNqQxmMmrMEW4iq6DLVr2UYJFA0rsnt7PcBxVv7AMdKuW8YVBxU1UdkKKaMS4scA8Vi3UG0niuxlQMprn9QjAJoMqsOU55xg02pZxhqhpHOLSUUGgDXhjJOTWpbuIwKpA08ORXrcqPzZYiSZri6wKikuiR1rP8yjfSUUip4mUlYleTcajJpuaTNWcrdx+aQmm5qKWUKOtIaVyG7cYPNYsx+c1buZ85qgxyahnXTVgoFAGTUyQk0FtiJEWq3FbUsMeDyK0oVGBTSMpTIY7X2q3HABUgAFOBpmLk2OVQKeKYKcDTJuSCnCmCnA0APpc00GjNAh2aM4puaYWoGP3U0vUZamlqAJC9ML1GWppNIokLUm6o80ZoAfuo3UzNGaBkm6jdUeaM0AS7qgnFPpkvIoGioOGq9A9UW4ap4W6UimaavUoaqitUqtTMyyDS1ErU8GmA6ikzRQA6jNNozSAdmmk0ZphNAxCajJxSsajJoGBNNJpCabmkMWikooKFpDRmjNIAppwQQQCDwQe9LSGkNHm3iTTE0zVGSIYhkXzEHoO4/A1jV1fjgj7baDuIj/6FXKV5lVJTaR69JtwTYUUUVmaBRRRQAUUUUAFFFFABS0gpRQA4U9RTBUi0jSJKgq5CvNVoxV6BeRTPSw0bs09MsZr+9t7S3XdNPIsSD1Zjgfzr6ltdPtvDug2ul2wxHbxhc/3m7sfcnJrxf4OaSL7xml065jsIWn5/vfdX+ZP4V6/rN0cNzVJG9f36safRHP6tefe5rhNa1LYrAHmtzV7zG7mvO9VvDLO3PFawVz3sPCNOHMyndXLSMSTkmqRbJpXbJqOtTmq1XJ3HE03NFFIyuLSilC1IqUFxjcaq1Mic09I6uQWxcgAEmpZ30aDkyKOL2q3FbliABmtew0OaYglCBXX6T4WDMuY8n6VDR1yqUcOryZyun6FcXRHycV2uj+FdpXKZNdKmm6fotp9ov7iK3jH984J+g71zGs/EdIFa30KHb2+0yrz/AMBX/H8qV+x5zxmJxr9nho6d+n3nTXT6V4YtRPqMoDYykCcu/wBB/U15p4l8XX3iGba4EFmhzHbIeB7k9zWHeXs97cPPczPLK5yzu2SarF6zlM9LA5TDDy9rXfNP8F6Cs1MEhVgR1FNZ/eowyswBOB7VlzHpzrq9kdR4fsY57wQRT2/2t1Eiz8sUU8YAxjfnr6V1/iDxGfCEENla7bu8mHmOXwFj55Y45JY56muG8LXKW2qwIZvs7PIoZsEmReu0+gzjp7VveONDuZ3XVbZWlhEYWReSyY7nuR71yytz2Z8/iaUZ4tQrv3TldX1SfV9RmvZWIaU9BnCj+6M9qgfS5X0cX6fMokMbKo+6PU/yqBlIQEjGenvVmz1G5swFjfdFkkxPyhJ9RW6T6HsypWpqNLp+RjSxZBHQ1X8lEUSSEBeOO7fSteVTKGkccZySBjHtWPJullJJz2HtWiueZiqKhJWWpEyec+VXC9hmrlrpTzsMKef1q3p1kZGUYyScAYrtLazjsF2YBm/ib+77D/GtIxuYzpUcPD2tbVvoZmneGIoUD3GFP9wfeP19K20hiRNixoE/u44/H1pQadmt1BI8LEY6rV0Wi7Ip3Ok6fdg+fZQsfULtP5isS68FWEuTbzSwH0Pzj/GumpKbgmc0a011OGPhnWNMl8+xnEjDoYm2t+Rq1H4tvrMeVqdkGkA4YqY2P17H8q64io54IriMxzRpIh/hcZFRyW2Z1QxN/iRlQeLdPOmC6kt5fNLbfKWXAH47easXPjmy1DSIrCe3PloCRhssrE9Rx09qzNQ8KxPbSPp6lZE+byM5D+u3PcelciqlZNuDnPeo5mtz0qUqcrSSPTNG8HPrtsl5ZypLbscFt23bjsc9K66NdP8ADGly2dlOlxfzr5ckkZysa98Hua4rQIvI0aBeoYs/Pucf0rT3VVicVUqVZcs5e72/zHu1QseaVjTao46lS7EoopKDC5geL03aNHKOsU4P5qf8BWHoN/8AYdcaAnEFyQp9ieVP64/Gum8RJ5mgXYx90B/yIrgLrOy0lU4LRDkeoJH9KylpK52R1gepj3p4rO0m+GoaZBcnG9l2v7MOD/j+NaK1qnc5paEyCrCrUUVWVrRI5pPUAtBSpEV3YIilnJwFUZJq4+j6kke9rOTHUgYJH4Dmi5rGmursZLpVWRcVeY9qqyipaNHFwZRcYNR5qWQYqAms2api5pM0maTNA7ik0maQmkzQNMbNBFcwtDOgeNuoP+etc/byy+GrzyZi8umyk4wOUPqPf1HeuipJrOK9haCVAyt+YPqKlq+xvTjfcnTbJGsiMHjYblZTkEVZTT72RN8dpcOnXcsTEfyqXRNLufAdk93q8sbNIM29kw3bP9s+h9qgufiRqsku6GVox6bun4U9TanSq1daKTXe5AykEqwIYdQRyKicV0+ja3aeMh/ZuqBEvSP9HulADA+h9RWBe2stldzWs67ZYmKMPcUE3fM6c1aS/q6KLUwmnvUZoOeWjEpKU02mSFFFJSAcDTg1R5ozQawnbQlzShsVGGpCaaYVad1dFoPS7hVQSYp3mVqmcLiWdwpjNUJlpjSUXEojpHqrI1Od81AxzUNm0URsajNSkE00qag1REaYVJqfYTTxF60ilFsrxxndmteywMVRwFqSOfYaZokonSwkFKfWRBfAY5q19tXHUU0dMKqsWpGAU1g6g4JNWri9GDzWLd3G4mgwrVLlCc5aoKfI2WqOkcwtFFJQBu5pc0wMCOKXNewfl4/NLmmZozQA+jNNzUckoUUDSuOklCjrWdcXHXmkuLjrWfJIWNQ2dMICu5Y01VLHFIoJNXIITSNW7DoLfpWgluMdKWGLAFWRVWOeUyt5WDT0O01MwyKhPBoJvcsqcing1XR+1TA0ySQGnA1GDTgaAJQacKjBp4NAh2aM0maQmgBSajLUFqjJoGKWphNITTc0DFzRmkpKQxaKSjNAxc0ZpKKAFpc02loAdTX6UtNc8UDRUfrUsJqF+tSRdaRTLynipFaoVPAp6mmQWFapQarKamU0CJgaWmA06mAtFFFACGo2NPNRtSAYxqMmnNUZpFCGkpaSgoKWkopDFpKcBS7aClFkdIakK0zHIFAWaPPfF83m666Z4iRU/TP9a5+tDWpTNrV657zMPyOKz68qbvJs9emrRSCiiioLCiiigAooooAKKKKAClFJSigBwqRetRipVpGsCxFWhAORVCLrWhB1FM9XCrU91+B9qI9J1y9I5Z44QfoCT/6EK6HWp8Fuay/g4AvgG/kUctfuCfoiVJrkpy3NaRRVN3xMmzh9futsb4PNcNM5ZjXR+IJ8sVz3rl3OSa6ErI9urO0EhhNNpTRTOMAKeopFFWIoi7AAZJpWNIR5mLHGTV62sJpyBHGW/Ct7Q/DE926F4yQeigda9W0jwXb6faC4vPLhUDJycY/GplJRNKmIpYb4tX2PMdL8H3d0QWTaK7jSvAyRBSYsn1IrV1DxRpGjRstlbG5lXuflXP1PJ/AVw2seO9Y1HdGlx9mhP8EHy/metZ8zZrSjjsYrU48se7O6ul0Lw+m7UbuNGXnyU+Zz/wABHNc1qfxIcK0Oh2a2qdPPlwz/AIDoP1rgJJSzFmJLE8knrTVdWbBYLweTWbmehRyWjB82Ilzv8PuLd9qF1qE7T3c7zSnqztk1RZ/fFN85VOXBZOhAOKqyTe5rNybPRlXhSjaCsiZ3wGOQQOMjtUazKWO5sAA446mqok3PjIGfU1XMuTxUnn1ca9y79oXGTknPK9Ka8wYjgEEZwOOapsSED5GCfxqdVBQNuHoR3osjGFeUnY0xdAWcZhmeJ0yrgdeeQQevtW94Y8W32lSKtzJJPYrhXVvm2g+h9fY8VySr7cVZto2klEauqlupZgq+vJNZuCtZnQ6ca0XGotDrvE914cvlWbTEdLkjkIu1OvIIPTv061zSrzU11araSRosvmbo1ckLgc+h7j3qS0gM8oQDJJrSlFJaM7cLShSpWTbXmSta7dHubhgMBdq5GcknqP8AGufhtyz13mr6dIdBSKFSQrBmH9fpWVoukiUvcTjFtFyx7Meyj3NaJXORTpzUq03oi9o9klhZC8fmaTiFSPuju3+FWA1JNM0r7mwBjCqOijsBUe6t4qx87ja0q0uaRYVqeDmq6tUqmtDyJEmaM00GlzQIWkopM0ikw6HI4PqK5zVtKR9RMsSjfOrPsA6sOuPw5/OuhJrL14SLpouYAxntpUmTaPfB/Dms5rQ7sJVcZWRq28Yht44h/AgX8hUmaghuEniSSM/I43Ln0qXNUTUnLm1FzRmm5ooM73FzSUUuKDSMGyjqw3aNfg/8+7/yrzmQ7re3H91WH/j2f616TqY/4ld7x/y7yfyrjtE0L+1xKzTeWkTAHC5Jzn/CsZq7O2FNqJBomrS6ZNyC9ux/eR/1HvXoMMqSxJLEweNxuVh3FYX/AAidiqbVefd/eLD+WKroNQ8OnOftVgTlgOqe+O38qcboU6XMvM7GM1YU1k2GoW99B5ttIHUfeHQr9R2qe91S102ESXUoXd91ByzfQV0Jq1zz3Rnz8ttTb1G/k0HwomoWwAubqVovNI5jUcfL6HivO4fEGpQXv2mK8mWUNndvOa6qwt9W8SaZLBdp9msFLPbQO37wue/068e9Zlt4F1ee52NAsMIPzTyttUD1rF3bPbwLo0qco1Wr9TsLyZNT0TTNaMIiuLoMk6gYDOv8WPesiXvWnqFxELaz0+2kMlvZpsEh/wCWjHq1ZMrcVotjyelltrb06FSaqrHmppWqszc1DLiKTSE0wtTC9BRLupN1Rb6TfSGiwprV0HYde08SY2G4TOfrWIr1ZhlaN1dDhlIYH0I6UHRHWDXcufEqSY+IZVdiQGOAa4XvXq3iKwXxjpcep2O03UagXEI+8reuPQ1562h3yzeUbaTdnHSkz1cvrQeGjDZx0aE0SSSLU7aSIkOsgIx9a7/x0FHiRmAAdoI2k/3sf4AVV8NeHI9GQaxrKhIYvmjjP3pW7ADvWbqd/LqV/PeTH95M24j09B+AwKZx4mpGtiFKG0U1f16FB6ip7mo6EcVR6hSUtNNBAUlLSUBcKQmg00mgLjgaU81Hmp4k3GkbwldWItjHpRsYVpxW2R0pzWox0qhOi2ZDEioyxq/PbY7VTMZBpXMvZu9iPBNKI6kCgUZFI2jTUdWN8sUvlinA08A1XKyXVgiLywKjf5atFT6VDJGT2p8hnLEx6FCRzUBcg1ckhPpVWSPFJoj2vMC3BXvUn2w461SYEUzmkUpFuS6J71VeQtTcGkK0BcbSUpGKSgLhSUUlAFqG7yBmrsc6tXPK5FWY7kivTTPzuVO5uhge9LuA71krd+9ON1x1quYy9ky/JOFHWqE9x71BJck96qtIWNJs1jTsPeQsaaq7jSKCxq5BDntSNG0h0EOcVoxRACkhix2qyBiqSOeUrgBinUlLimZC1C/WpaiIyaBoE61YFQqOamFA2PFOFMFOFAiQGnA0wUuaBD800mkJphNAwY1GTQxppNAwzRmm0tIYZooooGLRSZozQAtFJRmgBaKM0UALTZDxS1FK2BQNFdzzUsNVmb5qsw0i3sWx0pwNMBpRTMyVTUqmoAakU0AWFNSA1ApqQGgRJQTTc0ZpgBNManGmtSAiaozUrVEaChtFFFIYUopKUUFx3HiikooOuMVYDTDwc0+mkUjOaseWa3CYdavEYY/esw+hOR/Os+uw8aaa2+PUY1JUgRyex7H8uPwrjzXl1Y8smj0KUlKKYlFFFZmgUUUUAFFFFABRRRQAUopKUUAOFSrUQqRaRrAtRGr0B5FZ8Zq7CelM9PDPU+gfgxNv8C6rDnmO9LY9ii/4UuvkqzCsT4IX483XNMJ5lgS4Qf7pKt/6EtdB4jhILGt6RLlyYiR5RrjEzGsInmt/W4z5zVguuDXQ1oet7TmihlAopyrk0rCRLEm44Fdr4W8Pm4mR5EznoK53SLQT3SKema9p8F6arToSvAxUzdkKvW9jTbW5traxeG9KgeKJJL+5dYYFYcF26Z9gASfYVh+I713fa9w0mxQpdj1PcgdBn2rX1q5+0+JZZc/udMi8mMf9NpAC7fgm0f8AAjXB+IL0qcdSTnnpXNuznyzDyr1VN7swtUulLEA5bkD/ABrEdqmmkLuWJyTVVzUSkfexSo07DHfFQPLjvRK+Px6VTeXB68joajc8yviLEstxkDOOO/rUDSjYeTuz09qZLKZQznGRyT0zn2qszYHb6U0jyq2IZM0g796hZxn5cge9ML5GOhp3lHGSRn0FM5HOU9iVRvjycgA8mr1uVMfTjdz/AEqnCQAPVfXpVy0XCuG5wCQQM81LO7CR95MtRqNwJAYZ5HrW7caDEuif2vDLJHallVFuB8zsSchQOwx1PXmqtppjySWK7VnluTnydwGORtzj1HNeyx6Pp+q6F/Z88UTMgWF0UcI6g/d+meK5qlSzTRvi8b9XcGvn6Hjzzme0trcAFYQQGK/NknOM+ldFoOlHiRgM4zRc+GH0rXDahHa1RwY5X6v8oPbr3rQ1jUU0GwWOMg3ky/IpH3R3Y/0reDuvdNquJ9rGNLD/AGhNU1mLTrlbWFVmuiAGyflj+vqfajWJNoghAQFkE0gRQo3MPQegA/M1y+kKhvftNyDJglsMfvN71v6pMs10singxqD7EcY/St4R1ucmLwyo8sV835lFqbmhjTc1tE8WtIkU1MpqBamWrOGRKDRmmiigkdmkJpM0GgaEJrL8SXjW2ixxRnD3DlmI67RwB+eafquqQ6XAHl+Z2+5GDgt/gPeqDw3HiGztZHUW4RSDuBwRnIK9zWcn0R6mBSpv2k9il4a1hba6a3u5G+yuDycnyz2Ndcjq8ayIwZG6MpyDWRa6BYW6ENGJ2YYZnHb2HalXQ4Ldy9jPcWbH/nnJlT9Qc5qYqSHXqU6rutzXzRmsrdq9uP8Al2vFH/bJz/Sga3DHxeQXNo3rImV/76FVzJbmMaTe2prZqzaWs17OkFvE0krHAVRk1nRXltMu6O4iZfUODXe2kkPhrwwbiIo17crueQEHYOyg/wA/ei/Y6JN04pRXvPRGXq3hhLLw/qD3l1Gbk2shWBDnGF7muN+GqWVxcalZ3srRBkSRJF7EEg/+hCmSeJJp9Rea6d5InRo2VT0VhjisazK6XcvNaXLuzKVG6PbwfXk1nre53xwFfkcJyu317Hpeo+HLi2iNzBIl1bf89I+31FYUsaxozyMFRerHoKPC/iq5tr9Vmkyj8MvQEfStPxh4cVry1uoH2aZMhcoozhuPlU/w59veqMJU50aip1nvszhJVt5dSafRYpEniGXaPIQ/h0yfTv6Vf8OJYSvJcPJLPqYOZDc/fT/dHYVpJFHBGI4o1RB0VRgVUvbBLtlmV2guo/8AVzx/eHsfUe1K1nczqTT93Y31mI780552cfO5b6nNc3BrMlvMtrqqrBMeEmH+ql989j7GtUz+9axkmcM4NMtPIAKqSy1E82aryS0Ngk+osj1XZ6R3qFmqDVDi9ML0wtTC1AyTfRvqHdSbqALCvUyyVSDU9XoNYzsa1rezWkyzW8rxSr0ZDg1vJ421dUxvti2PvtAu6uQWSniSkaS9nPWSuat/ql1qM/nXc7yydAWPQegHQfhVBnzURfNJuoBzSXLEUnNJSZooMG7i02lpKYBSUU2gANNNKTTDSAUdav2q8is8HmtC1cA0GlLc1UGFFKaajAqKfTPRVrEE0YIzWVcYUmtO4kCqaw7uXLGkc1WSi9CNpOaVeTVdTk1ahGaqKucFWqyZEzUwjpUXAp9dEYnnTqNsbsFNKCpKaarlRnzsryQiqU0WK0zUEyAiolE0hUaZiyR81Ds5rQmj5qAJzWDR2xnoQCKlMVXUi4pzRDHSqUCfa6mU8eKhYYrRmjxVGRcVDRrGVyGkpT1pKRdyJ4iKixitaSEMKoTR7TXptH5/CdyHcRRvNIaSkajs5pVUsaaBk4q5bwkkcUJCk7DoIc44rTggwOlFvb4A4q8seKtI5ZzIwlOCVOsdSLFVGNyuEpdhq2IacIPagLlLy6YYjWiYPammD2oC5QCYp2KtGGmGKgdyAU4U8pik20AANOzTaKAFJpjGlJqNjSGhCabQTSZpFC0UmaM0ALRRRQMWikooAWiiigAooo70AGarTNU7nAqnIcmgqJCT81WYXqAJmpFUikWy8rZp+aqoxFTK+aZm0TA08GoQaeDQInU1MDVdTUqmgRKKWmg06mAUhp2KTFAETCo2FTkVGwpDRCaSnkU3FIoSgUUUDTHClpoNLmg6I1B1NNGaWkTKdyKaCO4heGZA8bjDKe4rz3W/DdxprtNCrS2ueGHVP97/ABr0jFGysqlJTRVKs6b8jxnFGK9Nv/Cem35LiM28p/ii6H6jp+WK5+48B3qEm2uIZR6NlD/UfrXHKhOJ3RxEJdTkaK6BvBmuKeLVW9xKv+NN/wCEP1z/AJ8j/wB/F/xrP2cuxp7SHcwaK3v+EP1z/nyP/fxf8aP+EP1z/nz/APIi/wCNHs5dg9pHuYNFbp8Ia4P+XE/g6/41E/hfW0GTp0x/3QD/ACo5Jdh88e5j0oqzcadeWv8Ar7WaL/fjIqtU2KTFFSKajpwNIuLLCGrkTc1QQ1Ziag7qE7M7j4f68PD3jHT72RttuX8mf08t+CT9OD+Fe5+KLEqWxyp5Br5iicEYNfQngXxCPFng+OCd92oaeohmB6un8D/iOD7itKbtIvGRdlVRwer2WXbK1zM9nhuBXpmtacVdvl71ylzZYJ4ruTugpYhpHK/ZiD0pyW5zWy9oc9KfFZEsOKDoWIJdEtyLhDjnNe4+CYQsTM38K15bo1jiVeO9ehapqieGPAl9dlgtxMnkwDuXYYH5dfwrnrPQyxFSVVKC3ZWtrpbzQvthCq9zNPM7L/ETKwH/AI6APwrgPEcimcYyW5DHdke2PSuj8N3Ql8FWQU5ESvEw9CGJ/qK4/WLjzrogKBtzyDnNcyep9LkuH5Z2fQy3NVZGwassOKpS9aze57+KdkV58M+EyMdAapTZUsDnr1q2+OckAdelVnlBwWG4qOpPWmjwK7T3K6N84z0zk/hVctzmpS2SegI6YqMMVbIAz7jNUeXNgWLtzk1aVgqDaQykkBWHK1XVD1I5q1EmI+2enSkzTDxk2yWFIuSOhByP/r1ftnKphXCvxj5en41Uij7c4Jq/FbneVPRe46VDPXwsJXSSNGNJRpzTBh/rR6bg+DyD1AxUmnaje6dcCW1uJUbOSA55+tVkQjtWnp2my3cwVEyT7VUYrqes6VKMG6trHf6Fqzapps17qmJpbZfldsKGGO56ZBrh/FEEYuV1IagtylwcDjAGB/D6qOlO8S6s9pbjRLQqIkAMzLySfT2rkZ7mRLVbcOpjyXC91PQ/04rJQ5ZXR5GHoqhN146J7LyLr6iAUSNtqgA5Awc455ro7e6F1YxSfxJ8rfjyD/OvPjKQc5rd0PVVhcxyEeW42t6j3FdEHZkVa/1lOD36HSmkpXBQ4PPcEdCPWk710o+aqyd7MelTCokFSCmYXH5pc0zNJmgQ/NBNMzRmgaMy60Gyu9TS9m8xmBy0ZbKvjpn0HsK1mbPWoyaTNTypGvM3uPzRmoy1JuoGiTNHBBBAIPUGo91KGoNqW42y8MWGraxaQANbNNKEZ4MDg+x4/Spdc0tvCqT6bbXsk1q/8DryGz19OlWtNvBY6naXbfdhmV2+gPP6ZrT+I+mSfaxep80LjOR056Gs7Hq4ab+swjJ+61+KPM260gNPkXDGmgc1nY+gadyeB2SRWU8g5FevXzGb4c2c0mS6TLjPocivLdKsXvryOJATkjOPSvTvE91BZ6BYaOkg87aJ2TPIUHAP5n9KpHkZu05UoLe9/kce7VGWprPTC1Wjzqy1FnjiuYGhmRZI26qwrIMN5pIzalruzH/LBj+8jH+ye49v/wBdauaTNJozjfYz4tZsp+BcKj90l+Qj8+P1qw0maxtd0cThrq3AEoyXX+/7j3q5YEf2RZMO8ODn1BOaE3ezHKKtdFlnqJmpGamE0zMUtTC1ITTSaAHZpN1NzSZoAkBpQ1RZpwNAXJg1PDVADTwaB3Jwadmo1NOBoC4+jNNzRmgLjs00mkJpCaAuKTTSaQmmk0AOJppNITTSaAuOzzViKQrVVTk1LnApG9JdTTiusDk1KbwY61hNMQetHnEjrTKnWtoi/c3We9Zcr7jSuxaoiDQc0p3Hp1q9BVBDzV6A1cNznqvQuj7oopAeBS11I89vUDTc0pptBIU1ulOpjHikxopTCq4+9U87YqmZMNWEtzthsXl6UGoEl4pWkHrVJ6ENO5FPjFZ8vWrksmaoytmspHRTIG60lKetJioN7mrjiqN2AK0D0rNumzmvVZ+dU9yietJig05BuNQdV7Ilgj3Gtm1g4HFU7SLkVswoAKtI5qsySOPAqwkdNQCrCAVRzNipFmrCQ0sYFWowKZLZEsFSC3q0iiplQUxcxQ+ze1NNt7VqiIGlMA9KQcxitb+1RNb+1bbW/tUL23tQUpGI0PtULRVsyW/tVWSDHakVczCmKYRirrxYqu6UDK7VG1SuKhakUhtFIaSkUOoptLQA6ik/GigB1JSUUDFopKKAHUlFITgUARytVU8tUsrVEgy1ItE8acVIY/SiMYFSUxXIduKASKlIzUZXmgLj0YmplNQoKfmgTLCGplqshqwlMlky08CmrUoFAhMUYp4FLtoFciK1Gy1ZK1Gy0DuViKYVqwy0wrSKTIMUmKlK0m2kO5Hiin7aNtBVxoFOApcU4LQFwAp4WlValVaAuMCU7ZUoWnBaLBci2Uvl1MFp23iky4q5X8uk8r2qV3C1GJQTUnUqN0N8v2pNlTDkUFaZlKPKQkEjB5HoayNR8NaVqSnzbVY5D0lh+Rv8D+NbZWk21LinuKM3HY8r1vwpeaQGmQi4tR/y0UYK/wC8O316VhCvbnjDKVIBB4IPevO/FvhtdOb7dZpi1dsOg/5Zt7ex/T8q461Hl1id1CvzO0tzl1NTI1VwakU1zHoQlYvRyVveG/EV54b1iHUrFwJE4ZG+7Ih6q3sa5lGqwklFzvp1E1Zn1Bpd9pHjnSftuluBMo/f2rn95C3v6j0PesLUdAeNiCmPwrw/StYvdHvo73T7qS2uY/uyRnB+h9R7GvXNF+M1hdwpD4k050lAwbm0AKt7lDyPwzW8KrW5zzw0o6w1RC+jvn7v6VNb6M5YfL+ldCvjTwBOm/8AtsR5/he3kB/9Bqhf/Enwbpik2C3OpzD7qrGYkz7s3P5A1brIiMar0UTc0nRrezge9vZEhtoV3ySyHCgV5f458Zf8JNrCpa7l0y1BS3UjBf1cj1Pb0H41l+J/HereKXEdy6wWSHMdpDwi+5/vH3Nc8j5NYTm5M9rL8NyTVSb1PSfAd6JNM1Kw5MgAnRRzkdDx+VZd+h+0MWUg5wc/p+lZfhfWP7F1y2vDzEDslHqh4P8Aj+Fela9oKTAS2/zo/K7PT2rO9tz3aWJjh695bSPPDgHkZFUJhhuenqK6htGeNpA8LM/OzHqAD+J/SsS7+aQr5EQJ6bBgfhUN6npzqxrfCYs2e9VfL3tjjHv2rQnRSflJ/EVWliZBxnPOccVVzxsRSblcpiHJJzuAHJHFHlBcjII7HFWlt2WXb6DjPen+VxjHJ68UXOZYfyKyRHuKuQQeYwXOM8D3PanRwMWxgfnxVu3g3tgFRjuTgUzuw+FuEcAQAjBB9RircMXIA7+tKsZJ55Pr1ra0rS5bmVQqE/h0qowuewo06EOZk2laM1zIuTkE/wAIq/r97HodsLCyIF1Iv7xwclB6fU1uzCPQNM3BkFw6/K74Cp7k9Pwrz+9vdLikeSfUTPKxy4hXcSfr0/WhnkQrRxFX2lV+4tl3MiRHYHGcGqklqwBJNaM3ijT4+IdM8xR3ll5P5CqE3i6E9NJgH/bRqnQqvjcK/iM6SNsnio1Zo2yODWpZ67p99dpBc24tQ52iUPlQe2c9B71qXnhpyxEbgkdQeDVKLex5l6E3enPX7g0TX0MYs73hB/q5e6fX1FdFtKkA4IIyCDkEeoNcHdaTd2eWaNto/iA4qzpniGbT8QzqZbfP3CeV91P9KuE7OzMMTR9rq9JfmdqKXNVbW9t72HzbaUSJ37FfqO1T7s1umnseROEoOzQ/NJmm5ooBK47NGaTFGKVzVU2GaQtSEUw0FcjQ4tTd1MJppagViXdS7qg3UbqRcdGWQ9df4e1+znsBo+tDNuBthnPOwf3W9q4gPUiSYPWpt0OvSpGzZ1WtfDlg5msSJYGG5XTkYrItfAl7LIF8on6LUQ1+/t7m3t7G8mgjto97hHOC7dAR9BnHvVmbxRrVwhSTUrgqeoVtv8sVKOyGKxcI8vMn5m/BZ6X4PiMlxsmvCPkt0IJz/tHsK4PXReatqT6ok/lXrd1OF29lx6f5NWGkLEkkknqTTC1DVzNSak5yd5PqZEGtywSmDVYxGw481B/Mf4VrJIkiCSNw8Z6MvINVb2ygv4tkq4YfccdVP9R7Vi28VxoV8juHe2bh1Viqyr3BPb+dTdopR9ozqAMjikIB6HNdFBqWg6DpcDmzM+oSRh28871TIyMDoeKLbxvY6g4t9R0u1mtzwfkCuv0I6VYlSrNOUINpf1ocs/61SRfJkeIf6uVi8f8Asv8AxL+PUe4rq/E2iwaa9vdWMjS6fdqWhZuqkdVNczKgdSpJGeQR1U9iPcGkZpqUbohJppNO3F1LEKJFO2VR0DdiPZuo/EdqYTTMJKzGk00mlJphpkhmjNJmkzQA/NKDTM0uaQEgNPBqIGng0ATA08GogacDQMkzSbqYWpC1ADy1NLUwtTS1AD91IWqMtSFqAH7qQmmbqVRk0DWrJEp7tgUAYFV5X5xSOh+5EQnJp4FQq1TKatHHKQ7bUbCpe1RvTsQpEYODVuF6osakjkwaE7MU1dGwjZFPzVKKbpVkOCK6Is4JxaY80hpMikzVEC1HI2BSs4AqpNLxUydioxuytcSVnvJzUs8mTVJ25rnkzvhHQtLNilM/HWqO+l30rlcpYeXNQE7jTN2TU8Me4iky0gjhLGrSWRbtWhZ2m7HFbMNgoAyKRvCm5HNTNtWsi4fJq9dS9qy5Wya9Js/O6URlTwLk1AOtXLdeRSRpN2Rp2qgAVeRwKoRttWpRJ71ojjlqaKyVOkorLWWpklpmbNZJferKTe9ZEctWUkqiWbEc3vVhJvesiOSrKS0yGayTVOsgNZSS1YSWkSaIwaDGDVZJanSTNAakbwAiqktv14rT60x4wRUtm8KcmYE0GM8VSljxXQTQCsyeHFCZTi1uY0i4qsw5rQmTFUpBQNEBpKcaaaRSCikopDHUUlGaAFopKKAHUUlFAC1G7YFOLYFVpHzQUkMY5NPiXmolGTVqNcCgpko4FOptLQQLSYzS0UAKBR3pRSheaAuPjFWUFQoKsIKZLJkFSgVGlTKKZI4ClxSjiloC40imMtSGkNAIgK0wrU5qM4qTaMGyErSbam60FaByi0QbaNtTbaNtBFyLbTgtSbKULQFxqrUqigLTwKAuOUU4CkFPFAXAClYcUtKeRSZtSepl3JINQxk7qvzw5qsse1ulSepGasWohxUhWmxYwKlIoOOs1ciK00rU2KQrTOe5ARUN1axXdtJbzruilUqw9jVoimEVLVyk7ani2qafLpepTWcvWNsBv7w7H8RVUGu+8faYZLWHUkHzRfu5P90ng/gf515/mvMqR5ZWPXpVOaKZKrVIr1XBpwNZnTGdi2stSCWqQanh6dzojWZeE1O873qiJKcHouarEF4S+9Txyc1nK9WImpHZRrts39LSO5maOR3VQjN8ihjwCehI9K9E8BeJ3ufK0K7O5tpFtJ1yAM7D+uD+FeVQuR0OD7V6b4AsIdMhXXL5TubIgU/3OjH8eg9gfWotqepNqpSaau+nqdJrNpcWyyMgKxsNpGM7l7gVxt3cN8sTxxCFV25dS3Tofb8K9HuvEGj3sHySr5LcHbyU98dcVzOo+H1mQXFo8dxbSjKPGc7qScXozbAVuRctZWZ59JGoJYrxnODS29k95vEaqzIm7G7BI9gev0rp4LE2U7mS3DqvzFZE4YDnv0rchtbSWwur2yhtVRTvUNCHIkOMjrkfyok7HXiK0YvRHnJgeKPY6uq5BBZMH2xUhtgm0jkMobnrXbXN5ezbYmhEeHzJgEhj0wQcjFZZ0eWaZm2Nknoe30q4xl1N6PJa9RW+ZgJF2xWnBDJcRxQ+SFVAeccsSc5rfsvDRdl+QlvpXRR6JZaVa/atSnitbdeS8hxn6DufpV2S3Ctj6FFe7uc/pHh0XEihl6mrut+IrDwjA1pYiO41MjBHVYv971PtWR4g+IqeU9l4fhNvCeDdOP3jD/ZH8I/X6V51PcbmLFiSTkk96HK55lSpUrvmrOy7f5lrU9VutSunub24eaZjksx6fQdh7CsmWWmyze9VZJKk4sRiklaIsktVnekd6gZqZ49Wu2OLV3fhHxB9rhXTbp/9IjXETH/loo7fUfy+leflqWKZ4ZUljco6EMrA4IPrVRlys4nUd7ntORj2rOu9FsrzO5PLY/xJ/hVbw7rqa1Z/NhbuIfvUHf8A2h7fyP4Vs10WUkdlPETS0Zyc2gX+nSfaLGUsV5BjJDD8Kuad4mAfydSQqRwZkXkH/aX/AAroKpahpVtqKfONk38Mqjn8fWocGtYnbCtGp7s0X4pI5ohLDKksf99Dkfj6fjUgFcS0d/od2CHZCfuup+Vh/ntXS6FrMGpXMNnco0MsjBFliG4En1X/AAoU+50fU7LmjsaqoWwACSelWv7Mvgm/7Fc7fXyWx/KumufEGieE7dIdPRJrnHzzlctn8en0qpY/ErzrkLcSSIpPXdwPwobZUKGInDnp09PP/I5h1wSMGoWFelXNtpfiuIplIb4jMdwg+8fRh3Fee3lrLZ3UttcJtliYow9xTTuZxtO8WrNdCi1Rk1I9QMaZzzjZi7qC1R5pM0EEm6l3gBmZsKoLMfQDkmos1T1G5UIlkMmS5ZUbnG1CRn8T/Kk3ob0029C5auXh89l2vOfNI9Afuj8FAqxvqLPJx07UuaSQ3UdyQvSb6jJozTFzslDVv+E7e1vfEVnbXkUc0Ds2Y5ACpO044PvXOg1YtbiS2njniYrJGwZWHYjpUtHRF80HFPcr+JIjDrV1Ht2BZCAuMAD0xWTEDvGM5r0XU4tD8VRJfS39vpmothJY5jtR29Qfeq1r4LtdLnM+tapaJboc7In3u/sAKV+57FLMaUaSU9JJbf5dyxqG5fhzpgmJ8xrtmjz127Tn+lcc5re8Sa6NYuYlgi8mytk8u3i9B6n3Nc9I1M8i7UW3o22/vIiWSQSIodgNrITjzF/u59fQ9jTZFVWBRt0bDcjYxkH19+xHrQxzSG7dFWIxxyRhi21h0z1wRyOlK2uhmpRasxhppqVfKlPyyCM/3ZTx+Df44+tMljeJgJFKkjIz3Hse/wCFUZtWIzSUZooELRmm5pRQA8VIKjFSqKCoq5Iop2Kci5qXym8vzNp2f3sHH50jqjSVtSsaaTUzgCoGoM6kLDS1MLUjGmE0GA4tSbqbmlUZNAIeoyanUYFNRcCh3CikdEEoq7FkkAFU3fJpJJCTURNMyqTuTK1Sq9VA1PD1SMGi5vqNnqDzKaXp3JSHM1IHwajLU3NSWXY5sVZS496yg2KkEtWpWMpU7msLj3oNx71l+bQZveq5zL2RdkuPeqcs+e9QtKT3qJsmpcrmkYJCSPmoDUrIfSoyKg1VhhptKaSgYq/erSs1yRWYvUVp2bYYUDW51GnwjaDWl0qhpzgoBWhjNB6VG3KeaXEhYmqZOTT5HyTUYr0GfmkVZEkYyavwriqkK5q/GMLTRlUkSg0uaYKdVnOyRTUymoFqVaZLLcZqyjVTjq0lMhltGqwjVVSp0NUSy2jVOr1UU1KrUEl1JKtxNms1Gq7AamRpTjeViS4uhAnXmsp9aw/3qTVnYIcZrl3kbfWO59LhqEeXY7W21BZ8AmpLiIEZFczpcr+YB711YG6EH2oWjOfHUYxV0YNzHjNZsq8mty6TrWTMnNani31M9hTDU0gqEikWmJRRRSKCiiigAooopgLQaO1Ru+BSGhkj1XLZNDvmljXJoLJIlq0BgUxFwKfQS2LS0lLQIWgUlKKBDhTxTBUi0ASJVhKgSrCCmSydBUyio0FTCmSFFFFMQU0mlprUjSG5G74qu0vNPmPBqk2d1SenSirFyN81OvNUojg1cRhQZVkh+2jbThyKKZwsbtoxTqKAuJS0lLQA4Gng1GKcDQMkpQaYDS5pDTsK4yKqOMGrearyrSsbxqsajYNWVORVIHmrMTcYpCk7ktIaWimSMIpjCpDTW4FIpFG/s0v7Ce0k+7MhTPoex/A4rxSRGjkZHGGUkEe4r3F2FeS+KbYW3iK7AXCyMJB/wIZP65rjxUdmd2FlujGzS5pM0ZrjO247NLmmZozQPmJA1ODVEDTgaRcZFhGqzE1U0NWYzQdlGepv6Bp0ms61Z6dGSDPKFJHZerH8ACa9H8TXUcDrawDZFGAiIP4VAwB+VYfwssgbu/1Vsf6LGI0J7M+cn/vkH86XXrnzbxm3dzVRXU+ryqPNPmeyRlTzZzk1Y0rUdRgMosb1oOhK7sA5IGSDx6Vi3E/J5qCO6khk3I2D06ZBHuKh6nRXxsPaWaujvbbxzc7dl5YwXCnoV+X/ABrq/D3iHT9TAtIrR7abaWZCgKMP94f1rymC4jnTLh43HGI0yCMdeT1z/ntXRadqb+HtGuLtiizSECAE8scdPoOp/wDr1ny3M61CjUoucdDstX8T+GtO1Ga3mknkmjOHEMQIDdxkkVky/ELRIubfTbqQ/wC2UQf1ry6a5eWV5Hcs7EszHqSe9Qmf3rVaKxw8lKK95t/M9BvvibqTgrp9vb2QPRwPMcfieP0rjdQ1W71G4M97dS3Ep/ilcsR9PSsxp/eoXm96CXWpU/hRZkn96qyTZqF5feoGkoOCti2yV5agZ6Yz0wtQedOq2KzVGTSE0maZyykBNITQTTaDJsuadqM+mXsd1bNtkQ9+hHcH2r1TStVt9XsVuYDjs6E8o3of8a8frR0bV7jR70TwnKniSM9HX0/+vWkJ23LhPlZ69mjNVbG+t9Rs47q2fdG4/FT3B9DVkGtzvpyuPeCG4iMU8YkjPVT/AE9K0vDXhSLSUutfMweCNWS2Vh8yuRyT9Af1rOQ12ehkah4K1SyHMkD+bjuVIH9Qaze9z1o1HGC10uk/Q8q1C7kuLhmYk88A9qqK5Vsg1avIGiuJEIIwxFVQvNZu9z6l3T906zwzrsttcxKzcKcD3zXXePoE+2WV6oAe4g+f3KkDP5EflXD+GNLlvdSgwjFAwJOOtdp47uVbULWyVgxtYMPjszHJH4ACrW54eYxj9Zhy72dzjpKrsankNV261aPMrbjaM0hpTs54f25AoMBpOKg19ktvEWnR/LujiiR8c/N0Of8AParAd1BCEIT/ABqPnH0Jzj8MVi6jpBZTNbtI7jllY5J+lRO/RHXQcEmm9Wbo44PanVUsLr7ZZxz5+Y8P/vDr/j+NWqpanPJWdgooopgLmnK1MozSLjJoS+jE72MTgmIu0kuO6rjj8c4p5mLEk4yTk1HK4e4bA/1USR/ixLn9NtMJqEr6nTKs9B7PULtmlJphqrGMqlxrGo3TKb/fB9v8/wBKeabuAjdcckjB9MZ/z+FBlciqWO5eNDGQskROTG4yM+o9D7jmozSUxpkzi1KF0lMJHVJeg+jf44+tRxoJc7ZYAB1LSqP68/hTCAwIIBBGCD3qKK2igLGJNu73zU2ZXMralzZbR/fnaU+kS4H/AH03+FL9pjXPlWcI4xmTMh/Xj9KrUtOxNy0LlCfntoj7oNpH5VNH9kcj95NGe4ZQw/MY/lVAVPH1ot2NqctdTrfDlhZ+Zd385ju4LS3MohPG5yQF3D061ny/ETWU1RpEkX7MPl+zhR5ZX0x6VN4a1S10+7mjvlY2l3D5ErKMlechsd8U2fwVbNe+cmt6YbBju8w3ABA/3eufapvbQ7qLoqUvbfK/9bljxPbWRh0zVrCEQQajC0hhHRHUgHHoOa5p62/EOp293LbWliGFhYxeTCWGC/OWbHbJxx7Vgu1M59oWf9diFzzTCac3JpRET2pnKyOpY1pwgPpUyxFR0pF046jS20VUlkyalnbAqoTzQVVl0EJppNKaaaZgGaM03NJmgB+6jdTM0ZoAdmjNJRQAtLmkpM0AOzTS1FNJoEOUZNWo4s9arRcmtCIfLVJE7jPs4IqtPb7R0rQVjnFNnTKUwaaZiOMGo6nnGGNQVA7hVq3k2kVVpynBoHc6WxvdhHNbkN6rgc1w8U5XvWhBfEEc0G1Oq4nNHk05Rk0wGpolzXoHwbdkWYEq2BgVHCuBUtWjkm9QpwpAKeFqjO4q1KopqrUqrQJsmjFWUqGNasotUZtkyVOtRItTKKZJItSLUYp60ATKatQyBetUwadv2jNDRUHZ3Jb4o6Hp0rAay8yT5Rmp7m6Znxmr+mru5NY2Z79DFKEdQ07TirAkYxW9t2x4pI9ijgCnMcinGL6nFjMZz6IzLlOtZM6VuTrmsydOtaWPNUjHlWq7Cr8qVUdaTNEyCkpxFJUlpiUUUUigooopgNZsCqsj81LM2Kpk5akXFD1G41ajTFRQrVtRigGxaKKKZAtFFLSAKUUYpaAFFSqKYBUqimIkQVYQVCgqwgpolk6CpBTU6U+mSIaSlpKBBTWp1Mc8Ui4uzIJBmq5jyasE5NOVM1J2QrWRXCYqRSRUxj4qNkxRYidTmHpJUwORVTpT1fFMxZYopoYGnUEhRRSUDFpaSjNAxwNOzTM0uaAH5pknK0uaQ8ikNFU8Gno2DTXGDUYbBpHRGNzQByKWqySjHWnebQV7JkpIFV5ZKbJN2zVcsSaQ+SwrNmuA8eQ7NStpv+ekOD+DH/Gu/VcmuQ+IkIFrp0uOjyKfyU1z4he4bUNJnBUmaKK887xaM0lFAC04U2lFA0SqanRqrKalVqDopzseoeBrprLwhfSBseddbcf7qf8A2VYuo3jO7EnnNaGnRSad4OtEl+UzbrjHcBsAfooP41zdxNvkOKd9LH11Gp7DBq28iJ3LtUsFu8h4FTWVk904CAsSeg7VNf6va6UzW1qqT3K8M7coh9AO5/T60kc0YwhH21d2X5l2OGDT7b7ReybY/wCFR95z6CsK91mW9vVnlVfLThIh91V9B7+9ZtxezXUplmlZ3PcmoC9J6nJicxdS0YaRRq3SFESeNi0EhIVyMcjGV+oyPzqkZqrGZioUsdoOQM8Cml6EcU8VzO5YMtMaSoN9NLUGEqzZKXphamFqbmmYyqXHFqaTSZpCaDJyAmkzSZooIuFFFJQIWiiigDX0DXZtFvN6gvbvgSxeo9R7ivT7W7gvLaO4tpBJE4yrD+R9D7V4zWxoOvTaNckgGS3c/vI89fcehrSE7aM1pVeR67HqwatDSNXudHvlurYgtja6N911PVTWLbXcN3bR3FvIJInGVYf561MGrZq57VKrFqz1TOzutE0XxX/pGm3KWl2wzJaTEDn/AGT3FV7f4Z3YfMgUKO5Irl99Pad2XazsV9CxxUWZ3QxVenHlhPTzVztp9S07wxaeRp5hnv1G3enKJ7k9z7CuKnneaR5ZHLu5LMx6knvUReoy1NIx51G7vdvqI5qE09jUZqjlnK7ENNpTSUEi0dOhwaSigCuEFnNJOi/uZTmZFH3T/fA/mKufiD3BByCPWmVCCLXrgQE8/wDTMn/2U/ofY8RszZe+vMtUUnTrRVE2YtCqGYAnAJ5PpRVe+k8rT5iv+skHkoPVm4/lmk3ZGkINuwlu/nW/nkYM7tLj0UnCj8gKkNKYxEfLX7sYCD6AYoxSWgTTuMIphqQ000zMiIphqUioyKAIzSU8im4oASkpcU4AlSccDvQAzFFOxSYoAUU9TimYpaClKxYWSnmWquaUtSsdCrWRIz1EzZppakHJosZyqXJ4Yt5rTgs8gHFQ2UeSK3YowqDig1o01IprYjHSo5rXavStSmSqGWix0ukktDk7uIgmqLDBrfv4gAawZeGNBwVFZjDTDTjTDQZiGkpTTaBXFopKM0wuOFFIKWkFxaKKSgLi0w040w0CHo2DV+GUYrMzinrKVqkI2FKnnNJNIpXFZn2kgU03BPei5SkPmjDGqrxEVaSTdTmQMKkuyZn4xRU0seKhpkMUGpYnIYVDTkPzCgSKC8mrsC9Kpx8mtG3HSu+J8RUehaQYWnAUqipFWtUcbY1VqVUzUkceauQ2xbtTJ1exVSI1MkRrRSyOOlSizI7UxOEkUkiqwkdWFtyDUqw1SRi3YhVKkC1OIqXy6dieYhC04CpfLo2UWGpEYqC6l2RkZ5qaVxGpJrGurnzHwDUSZvTi3qJGDJLW9Zjy4xWVZQ5wa11OOKUUVVn0RdSSplfNUVap0aqOVskkGRVCdKvk5FVpVzTHFmTLH1qo8JPatkw5NRtEo4NZtndSoymrmE8JFQsuK3JLcMOKoTwbe1K5U6ThuUCKSpGXBpmKDNMSg0YpDQMrzd6qgZarUwquo+akaLYtwjipqjiHFS4oIbCilxS4phcQU6gClAoFcAKcBQBTwKABRUqimqKlUUCHoKsIKhUVOlMlky9KdSDpS0yBKKKKBidqikNSnpUEh5oKQwdanUYFQr1qcUiri0hANLTaBXImTFMxVgjNRstIpMarYqRZKixSZxQMtbqQsBVYyYpjSmgfKWi4o8wVTDE04E0DsXAwp2RVPcRSiUikFi5mjPFVBPSmfiguEbsdKRVVnwaWSXNV2bJpHoU4aEnmkd6XzjUFFBtyon35qRBmqwODViI0iJR0LSLgVyXxEX/iTWbelwR/47/9auuB4rk/iDzodt7XP/sprGt8DMqatNHm1FFFeadwUUUUAFLSUuaAHA1o6JZDU9as7IsFWaUKzHsO/wClZlT21zLaXMdxA5SWNtysOoNBcJJSV9j0bxNftLL5SYESDYqr0AAwK5Vcl81qPfC80e3unijLuCr7Rt5BPIx+FU/KRbR7tn2RowU7hnk/ShvU+prS5+WS2tf5Gkl0dL0O5vUbbKw8uIg8hjxn8sn8K4ndWrrWqQ3UNvbWxJjjyzkjGWP+AH6msXNNnkZlilVqJRekVYk3Um6mZozSPO5x+aTNNzRmgXMOzSZpuaM0C5hc0ZpuaKBXFzSUUUCCkoooAKKKKACiiigBaKSloA2dB16XR7jBy9tIf3kf/sw9/wCf8vSbW5hu7dJ7eQSROMqw/wA8GvHRWxoeuT6RcZX54H/1kRPB9x6GtYTtobUqzg7PY9QzRmqtle2+oWy3FtIHRvzB9D6GrGa2PRjUutBSaaTSmkoHzMaaYakNRmgLjTSUppKBhRRRSGLS8EYIBB4II4IpuaeoyaRrDVlGSU6W6iVSbFziJgcmL/ZPqPT2rSiUTIrxESI3Klec0v8AZx1NRZqpZ5SFQAZO7tXc6B4Zj8CWD3epTxvfSciFSTHD9PVves9U7HY+RJdZPp3OctfDOrXke+HTrll9fLKg/nisbVNF1W21i3S70+5gghO8F4ztJ65yOPTv2rrNT+IFwHKQuT75ziqFj481GK6VjcMVJ5QjIIoaudVLC4r4uVGJ5dNZcV395pll4m0577TYkh1BFLvCgwso74HZv51wsi1SOZpTTVrNboqkU01I9RGmcklZjT0phFPNMNMi43FJilNJjccevFADyiRcSKxfGdmcYz6n+lMeRn44Cjoq8AU+5ObuY9y5z+dRVKG9woopKoQtLSUtABTTTqaaAuNNKv3qQ0gPNILmxYt8wreQ5QVytrNtYVu210CoGaDtw9RLcu0jHApPMXHWqtzchVIBoOuU0kUNRcYNc/KfmNaN5cbyeay3OTQeXUldjTTTTiaYaDO4hptLSUCuLRSUlArj6WmilFAXFoopKB3A00nmlJptAXA0006mmgVwpppaSmFx6Ng1aR8iqVOR8GlYqMrFx03Cqkke01ajcMKc8YYUFNXM80q/ep8sZWo1BzQZlKIZNatsvSs6AZIrYt04FehE+HrMnRanSOmotW4o+lbJHFKWpLbw5I4rVSJII9zdahtIhkVJqZKx7RUyO7BwUndjft6BsDFXbedJsA4rlmZs1paZI3mAc1J6VSjG2x0X2cHkCgQY7VZgG6MZqTZW0Nj53FRUZWRT8n2o8r2q5so2VZyXKRippjq6UpjJikxxZzmrlkQ4rCtA0s/NdBrIyprJsI/32fesXuevTVoXNy2iCR/hU4pwXCL9Kaa0SPPnK8h4NSq1V84pytQSXAcimkZqNX4p+4UMcVqNl+SMmudu7xxKcGt65kUxlc9q524gZ5DgcZrBn0mDS5VcmtLtmIBNXLiMFc4qpZWjBgSOK050+XFKIsby2MOWPk1CVrQkjyartHWtjxeYqbaQirBjppSlYaZSmFV1HNXZ14qoo+akap6FuEcVLikgXip9lFiGyLbS7al2UuymK5GFpQtSBKcEoC5GFp4WnBacFoFcQCngUAU4UAOWp0qAVMlMTJx0paQdKWmSFITS0xjikUhGaoGOTQ7UwHJoNeUljFS1HGKlpEMKaacabQIKSlpM0DEKg1Gy4qWkIzSHcqstM21aKUnl0F8xCqVKI6kVMU+gXMQFKjZatmo2AoGmVSDTGJqwVFROoFSdNJ6lZmNJQ4waSmehHYWlpKKRQtSxtg1DT0PNAF5W4rlfiAw/sa1X1uCf/HTXRK+K5Lx9PutrCLPO92x+AFYV3aDMox99HCUUGivNOoKKKKACiiigBaKKKAOq0/5/CsZ7rcOv6KaW4G7wxe+0sZ/nTNDJl8OXsQ6xTLJ+BBH9KsRp5+ianCOvlCQf8BOaD6GPv4aNv5X+FzkKSg0UHzwUUlFAC0UlFAC0UlFAC0maKKACiiigAooooAKKKKACiiigAooooAWjOKKKANLSdXuNJuvNgOVPDxn7rj/PevR9N1O21S2E9u3T76H7yH0NeTVe03Up9Oulnt32uODnkMPQj0rWE7aF06rh6HrFJWdpOs2+rW4aMhJgP3kRPI9x6itGtz0IzUldCGozUhqM9aRaGmkoNNzQUOpKM0lIdxRU0YqEVPHSZvR3Oz+H1mk+vG5kGRaRGVQf73QfzNYnjbWpbnU5IVY7FNdD8PpALzUYgcM9ruX32tz/ADrh/E8bJrMwbNZvdnrZbBSxcm+iVjDZiTQrYOaCKAKzvqe1zPmO38CarJb6rEm7uMe4qbxnpyad4iuPKGIZv3qccDPUfn/OsjwbbyS65DsByGHSrfxFtr2XxhcPb3uxVCrgMRt+Ucce/NaXaZ4+Ngli7p7x1MVzUbVTWHUEPz36n6xBv5in5uR/y9If+3Zf8aab7Hl1Yq+5MaY1R7pwebhCP+vdf8aTzZh/HCfrbj/GndmfKu5LHHJNKsUSF3Y4VVGSTV61sES/iS5ng4dQ0avluvPQYyOuM84xVKGW9AkW3uLdJJEKAiPYcH0NYcT3VrqCGUOkiOCQ3BqXJ7HXRoU3Hmbua8kgklYqCqg4UHrgevv602llZHuJGjzsZyVz1wTTatHHP4mOpKKKZI4UUgpaACmmnU00ANNNNONMNADlcqatwXZU9aoGnR/epFRbTNsXp29apXF2WJ5qEk7aqyHmhG1SbsEkhY1CaU00mmc7YGmGlJphNBLYUUZpKAuLSUUlArig04GmZpRQFx1FJRQFwNNpTTCaAuKTSUmaM0CuLSUZozQFxKSlJppNAXJY5Npq7FIGGKy81PDIQwosVGdjRMAcdKItPJccVcsU83Fb0NmoUEiixpa55/aR5wcVsQpgClgsCg6VaWLHavSifAV01uEaVehSoYkq9CnStUjgky5arg1aurUTJkCo4E6VpRjIwaUo6HThsT7NnJ3FmY26VoaVaAkNirGqIF7UzSrgBwtZcrPVnik4XRvooVQKKTOaK3irI+er1OeVx1JRSGqMAqOQgKSaeTWdqF0I4yAaTNKcXJmLqs4JYZqlp8gEo+tRXcjTOcVFDFLGc1hrc9xKPJY69MNECPSmMKx4L+SIAHNXE1BHHzDFaKR51Sk09CwaM1F9oRu9Me4RB1ptijSlJlrzMDk1XmvgBhTVCa73cA1AoaVqhu5v7Hk1ZcEzSt1NaEFqGGSKr2lttGTWipwMCjluWsU4aIURLGOKryjNTk0wjNNRsZVMTKe5QeOoGj9q0WSomjqrGCkZ5j9qYY6vmKmmKlYpSMe5TFUlX5q17uLis9U+eoaNoy0LVtHxVny6W1j+XpVryqpIhyKvl0eXVry6Xy6LE8xV2UuyrOykK0DuV9tGMVKRTDSKQ2ig0maQxwqZKgBqVDTEy0vSnUxDxUoFMkSonFTYpjLQOLKjrTVXmrJSk2Ujbn0EQU+jGKDQQ2JSUtNpALTaU0lAwooooAWigDNSBKRSi2NopxWmnigbi0IelRMaV5AB1qrJOKASJGfFQvIDVZ5SabvJqTpp6MexyabmlAzQVNM9CL0DNGabzS0ix1SKtRjrUysMUhNpB0rgvG9x5mrRQg8RQj8ySf8ACu9JGOuPevKNYvPt+rXNyPuu52/7o4H6CuXEy92xNPWVylSUUVwnQFFFFABRRRQAoopKWgDpfCbbzqNuf47csPqP/wBdXdIYNePbN92aNom+h4rK8JShPEFujfdmDQn/AIECB+pFXGY2mqK/Ta/NC7HvYOf+zxfZtfecxIjRyMjDDKSCPSm1r+Jbb7PrMrj7k4Eyn/e5P65rIoPFqwcJuL6CUUUUGYUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAtFJRQBcs7yW1mSWJykinKsK9B0XX4dUjVHxHdDhk7N7r/h2rzOrFtcPDKroxV1OQwOCDWsJ23HCcqbvE9bNRsaxND19dQVbe4IW5A4PQSfT39q2Sa3Wp6NOopq6EJpKKSkaXFoxTlGalWPNOwOViICpV4qQRUvlY7UNFU6qTNDRdUk0jU4L2MbjGfmU/xKeCPyrrPEnhq18Q2S6tpLCRHGTj7ynuCOxrg/u1f0nWr/AEe582xnKFuGQ8q49CO9ZOL3R6EKsozVWk7SX4mJcaRcwSFWik4OPu1JaaJd3MgVYX57kV29v4/0zUBIb/SZFkjkaMvbMMMRjJwaJ/HdpboRpmlBZD0luGDY/wCAj/GpVux6bzSrb+Hr66FvRrC28G6d/al+FNwwPkw92bt9PrXEXt3JeXUtxKcySuXY+5qrqd7d318+ovPJPOR+8jY8Oo/ujsR6UwyK6K6MGRhlSO4prVnBOTbdSbu3/VhkhqE05zTDVo4pyuxpptDU0mgzuLUq3DgAMscqjGBKgbGKhzRmgak47En7luzRnuR8y/l1H60jIUIzggjII6H6Uynow2lGOFPIOM4P+f8APFAXuJRShdxAVlJPQc005BIPUcUALS5pmaXNADs0hNJmkJoADTDSk00mgQhp0fWmGnxdaCobkx6VVc/NVpvu1TkPNJGlQaTTCaUmmE0zC4E02gmkzQK4tJmikzQK4tJRmkzQFx1GabmjNAXH5pM03NJmgLjiaYetBNKg3NQABCad5Rq5FDxnFSeWpOKDRQ0M0gjrTa0JbXI4FVGgYGghqxCTTCaseQxpPs7elArMgqeBcsKT7O3vVy0tzvHFMLM3NJizt4roBwMVnabDsUHFaJ61VjeOxg29wj4DKMmp5YgORWRGxibJ7VoR3quNpNd0dD5DFwTiSxpzWhAnSqkIDHitS3TpW6Pn6isy1DHgCrargVHEOBU1UYXM3VI8xZrFsXMdxj3ro7xd0Brl/wDVXX41nI7aMm42OwjbcgPtT6q2T77dD7VZrRHHNWYtBNFQzzLEhJoJSbIrq5EKHnmuaurhp5CB3qW/vGlkKg1Lp1iZGDMKh6ndCKpxux1hpgkwzitM6VDt4HNXY4wiBRT8U1FIxniJN6GFPpPXArMmsZIycA11rDIqpMgPahxKhXfU5JhLGe9QyzSAc5rori3U9hWVdwJtrOSaPVwk4t6lCBi781uWkSjBxWPCgR81r2sgzjNKO5eMceXQ0RwKeDUYORUgrU8RsWilxRigVxuKQrT8UlAXIylNMdT0lA0zMvI+KzUj+eta7Oc1RRcvUtG8XoXbWP5ateXTbdcLVimZtkPl0FKlppoEmQstRNUz9Kgc0i0RMaiY052qFmqWaIUtTd1RlqbupFInDVIjVVBqRDQOxoRtVlTkVnxvVuN6ozaJ8UhFKpyKCKZJGaaaeaYaRSENNNKaaaRQUlLSUDEpKU0UDCgUUoFIaJEFSFgopE6VTuZdtQz0qFJNFhphVWWf0qp5pJpeWoNatFJDXlJ71AzE1MYjTTHig4HZMgwTT1TFPOBTS1AKRIMCl4qDdS76DaNVolIFGBUW+nB80jX2zGucGkEmO9D81CetIXtLlLxDqX2LSJdrYllHlp+PU/lXnFauv6n/AGjfnYcwRfLH7+p/GsmvOrT5pHdSjyxCiiisTQKKKKACiiigAooooAsWdw9rdwzxn543Dr9Qc11muxRm6WaLmOZRIpHo3P8AX9K4wV2UJ+2eFbSbq0BaFj9Dkfo36UdT1ctlzRnS8r/cUtaT7VoNndnl4HMDH2PK/wBa5k111uhudLv7MjO+PzE/3l5/lXJGgxx8ffU+6EooooOAKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigAooooAKKKKAClpKWgCeGYxsCDgg8Gu00XxALoLb3bATcBJD0f2Pv8Az/nwlSxylTWkJ2FGUoPmieq0o61zOi+INyi3vX9klP8AJv8AH866ZRzg1utT0KdZVFdE0S5q7HFxUEC5xV+MYFaxRnVqWEEYoMYxUtFXY51UZRlTFVJJPIV5f+eal/yGa0pVyKytQjL2xiBx5zrF/wB9Hn9AaxqKyPQw1RtpFO0Q29jbxEfNsDPnuW5/rU2+iZt0rN0BPFR1lFWVjtlVbY/ec5HBqFT5DkZ/cSNx/wBM3P8A7K36H60+kIBBVgGUjDA9x6UNdiVPuK2QcEc0wmmKXV3hkbe6AMrd3Q9CfcYIPvQTTTuRJNMCaaTSGkzTELmjNNzSZoAfmjNMzRmgB+aM0zNJupBckzRmo80bqAuSZpN1MLU0tQFyQtTSaZupu6mFx+afG2GqHdQGwaQJ2ZfzlaozcMasxvlaiuEzzSRtPWJVJppNB4puao5ri0maTNJmgLi0UmaKAuLSUZooFcTNIWpSKaRQFw3UhakINNNAXHZqaE/NVenI+DQCZsrzHx6VCm4SUyG4AGCakMyjmg6IzVi7uXZz1xVR2TPWq010egNU2nJPWgzlPU0wy0u5ayvPb1pftDUrB7Q1cpVq1K7xWB9pNW7S5O8ZNFh+0R3FmQU4qyaytMn3YFa1WjWLujlpow44qqYnRsirMb5NWo0Vuor0FE+Bnir7le2umjIz0rfsr6N8Anmsw2AcZUVCYJYGyM1Sujnmo1Dso2BGQakrlrTVHiYBq3ra+inXjg1akck6ElsWZV3Rt9K5e+hZZ9wHeur3KFOelYt/5e44IrOUtT0sHhZNalzSMtCBmtQx1zVvqKwDGavR6urH71Tzs6amWqWqNKRhGpJ7Vz+o3xdioNW7y9EkfymsuG0e4mzzVc7ZzywXsldjbO1aaUEjrXT28CwxhQOaZaWYt4xxzVoCtIrQ82tUu7ITFFLSVRyjSKryirRqvLQUtzOmHBrDviQTit2boawr4Zc1Ejrozaehmhm3VftpSpGaihiDNzV37NtAIFSkbzquW5fgl3DFXFrNt1INaaDpWiOSe4/FFLRQZ3Eppp9IaATGU12wppzcCqFzPjgUjSKuQ3D7jTIEy1Rgl2rQtou9I0eiLMS4UU/FL0FMaQLTJUXLYdio2pPOU0bgaVyvZyW5G9V3NWHqtJSGiu5qBzUshquxqWaIQmhRmm96lQCkzanHmY5UqQKKieUIOtRrc5NI9BYZWLg4qZHqsj7hTw3NNM4a1PlZfR6lzkVRR6nV6o5WiY1GaduzTTQCG0004ikxSKQlJS0UFDaKdikxQAmKcOtGKWkNMlXpVK6iLdqtKcUNhqho9HD1rGWITnpVhUAFTsoFQyNig1q100RSECqztT5HqszUzgbuwLUwmkLU3NAD80mabmikUKTTkbmoiacp5pDRMTXK+JtaESvp9s37xhiZh/CP7v19fyqxr3iBbJWtrVw1yeCw6R//AF/5VxDMWYsSSScknvXJXrfZid2Ho/akIaSiiuI7QooooAKKXacZwcUlABRRRQAUUUUAOFdd4OYz22oWTKSjIHB9COD/AD/SuThjeaVI41LO5CqoHJJrtY7iLw/5NhEwd0Ia4IOQXIwwH0HH4Z70HpZYmq3tHol+ozSMR6lCH6LMEb6Hg1yN7D9nvZ4Tn5JGX8jXYzKINZfHRwJF9+9c54jjCa/dsM7ZH8wEjqG+b+tB0ZlTtTT7Oxk0UUUHihRRRQAUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAUUUUALRSUtAEsUpQ9a63QdfEWy2u2/dDhJD/B7H2/lXG1LFKVPWtITsTrF80dz2OAjANXlbivOfD/AIjNmVt7li1v2PUx/T29q72KZXRXRgysMhgcgiu2Ek0W6nOi3mjNRBx60GQetaAosWQ8VnXZzNbr/d8yQ/gAo/VjVqSUAVTmkV3bbglECNg9Cctj8sVz1HfQ9LC0pblV+aZTmptQdDVgpDS0lAipfpI9qXgYieL54yOpH8S/iP5U23uFuIRIvBP3l/umrRoEidJIlYZ5YcN+ff8AGptZ3RakmrMhJppNTvB8jSRMJIx1IGGX6j+vSqxNUZvQXNJmmk0maBXHZozTc09ULUDEpKtJbk9qcbU46UDsynmm7qnkgK9qrNxQJ6C7qQtTCaYWoJuSFqTdTN1JmgLkm6k3UzNJQK5bhk5xVlgGWs5MhqvxtlaRvTldWKcybTUJq1ckYqnmmZT0YtGaTNFBFxaKAKkVc00iXKw0LTglTLHmplhq1EylVSKnl0hjrQEPtSGH2quQz9sZpjphStFofaoHi9qlxLVVMolabVl48VCy1FjVSuNVyKcZWqOigq4pJPWm0tIaQCUUUUwuFSxNtcVFU0UZJpAtWdLpU3K811CHdGDXFWL+URz0rfi1FQoXNO51RdkZER5q/AazozzV+A9K9WJ+aTNa37VdNqkyYIANULc9K1YTV2MeZpmHd6U6nKj8qrQ/aLZuc4rrdofgjNZ+o28ccZYCsZqx6uDftHZmbLqzrHtzzWTNdSSNksabcNmQ1DUHspKOiHeY3rSiZweDTKSmHMy7DdsCAxyK6jSJY3TjGa4wHFbWj3JSUKTSIqrnjZnYMPSm0iPvjBozW0HofMYmnyyYtJRmirOQKgk5qYmonxjJpN2OijSc3oUJl4NYV4p3Hit6WePJWs67iWQErWXPc9H6o4q5m2/DVrxoGQVjqpjk5rYtHyuKuJyVE0Sxw4NWVGKQU4VRzN3FopM0UyRaQ0tV55goxmkUlcZPMACAayZWLtU8khc0+G3LnpSZtHQbawFiDWqibFAohgCKKlYYWiwua7sVJ5tg61lzXmD1qe9cgGsSRyz1nJntYWirXLy3vPWrcN0G71h1LHKUqbnTUoxaN/zVI5NVpZkHes03DHpmml3b1qrnlVKaiyxJOtVnnFRsrH1qMxsaTISQ/wC0c1Ilwcdaq+U2anihNI6aLSYruWOaYp5qdoMikSE7uaR6kakbFmE/LUhbmmL8q4ozzTR5uJkmydWqVXxVUGnBqo4S6slP3iqQk96cJfei4WLe6jIqt5tL5tA7FjIozUHmUeZQFiaiofMo8z3oGTZpC1Q+ZSF/ekNIm3UhkqAye9MaSkykSvJxVaSSkaSq7v70i9WDtULNQzZqMk+hpXKSFzSZppOOvH1qN7mGP780Sf7zgUm0Uotk+aQms2bXdOg63SufSMFqx7vxaSCtpb/8DlP9B/jWcq0I7s1jQnLodJLNHEhkkdURerMcAVzOq+JncNDYEqp4MvQn6en8/pWDdX1zeyb7iZnPYHoPoO1V81yVMQ5aRO2lhox1eoE5OTSUUVzHUFFFFABRRS0AKGYYwxGKkUpJw52sf4+34iowM1oxaNceWJbkx2sR5DTttJ+i9T+VBcYSlsihJC8JAdcZGQexHqD3pmK3rZLBUaB7wSxn+F02jPqDnI/KnRaDaS3St9txbZ+YYy4Ht2P1/Sg3WEnJJx1+Zz+KciM7hFBZmOAAMkmtybw9EGc29/GwyfLVlIZh2/E1pW0Vp4bt2OVm1Zhgv1W39h6t6n8BQVHBVOa09F3I7exTw9AZbgg6i64VAf8AUg+v+1/KssFpZC2fck9B+NE03mEyzOVT1PJaqFxdGX5EG2IdF9fc0G1WrCmuWOyOoupg9npd6pz8piY/7pI/lVHxVAPMs7pc7ZIdpPup/wACKTTZPtPh25gz89tKsoH+yeD+uPzrReEat4amgAzPa5ljHcgdR+XP4UzsqP6zQfdpP5rc4ykpTSUjwQooooAKeUAUEk5PakVSzBVGSeAKWQ/dXuoxQAw9eKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigAooooAKKKKAClpKKAJY5CprptB8QvYEQzEvbE9O6H1H+FcrUkchU1pCbiRKPVHr0V0ssayI4dGGVYHgipfMzXnWja1JYSBSS8DH5k9Pce/wDOu7tbiO4hWWJw8bDIIrq57q56GDcajs9za07RbzVkkki8uOCPh55m2oD2Ge5qCDwnqNvbatdK9vdRC4En+jyb2C4OSR6dP1ra8Tah/Z/hbR7G0ysbwCVmU/eZup/mK5jwtf3dj4htJLaQqxkCsueGUnkGsJO7R9HRwspUHUX3ehVdaiIwa3PE8EFr4k1GG3AEKTsFA6Dvj8M4rEY81SOGola6G0GjNNJqjmYhNRMaexqJjSJFSV4nDoxVh0IqQql3kxqsU/8AzzHCv/u+h9vy9KrE0wmiw0wIKsVYEEcEEcikoa4mlm/eqZUUbi38WO43YNTbrF+jXMZ9wrj+lK5Th1TI0XJrStrctiobe0MrDyJEmz2B2t+R/pWzZwFTh1KnuCMGmXTptsfb2QwMirRslx0qzGAMKBkngADk1rf2Bq5gMo0+XaBnHG7/AL5zmpueh7OEV7zORubHg4FYd1AUY12TruBBHPoawdRg5OKZhXoqOxzj8GmE1ZmhO41AYm9KZwOLGZpM04o3pSBTnpQSORNxq5FaFu1FpDuYcV0NpZggcUG1KlzGSmnk9qka0Ma10iWqAdKjntVKHAoOz6u4q5xd2CDiqVbmo220msRxtag8+qrSCnAUwVKgzTMmxyLk1ajjpsSZq7HHgVrGJy1KlhEiqYJinAACitlE5HNsTAo2iloqibjCgqJ4s9qnpDSauNSaM+SLFVJExWs6ZFU5o6xlE6qdW5msMUyrEi4qu1ZNHXF3DNNJopKRVxaOtJViCEuRQNK4kUJY1bVAgqdIgi1UuJguQKRtZRQ97jZ0NRrfMD1qmzljTKDFzZ0sZ5q7CeRVFKsxNgivVR8BJGxbt0rWgfgVhQP0rUgk6VojmktTWjPSqGsHERqZblUGWNUdSu45kIU81jUPXy5WZzEv3zTKkmHzmo6k9iW4lFLRTEAq3aSFJAaqitCwtGmfvSY0bMOqFEAzTzq59ai/sh8d6adIk9DTjc8bFezcib+2T60f2yag/sd/ekOjuPWruzi5aZP/AGwfaornVSYzg1F/ZUoNRXOnusfeolc9DCKCehnSXjs5Oat2lyXIUms6SB1fGKt2cTKwY5qT052sWrpQpzTrKXDgZqC8m4qvbzYfrVxZ4uIhd6HTA8U4Gq0EoeMHNSlwO9annOLuTUZAqq12i96rSXwPANFxcjL0kwUcGs6eUsaiactTo4zIRQaJWFgiLt0rXghCgHFR28G0Dirf3RRYiUg4pkjKqnJqtcXITODWdLdluAaGOEdbkd/IvNYzH5jV6ZXk9arNbMO1Ys+gw00o2IqeibjSLC5OMGtO0tCSMikkdFSooxGwWW/HFXP7NAHStK2t9oHFTvHWiieFiK15aGG1iB2qFrQDtW08XtUEkNOxgqhjtAB2pm3FaTw1XaKpaNIzZXzScCpGSmFaVjdVpWGk0CjFIaCHJsXNG7FMJqNmpAT76PMqsXpu+gqxb82l82qe+l8ykFi4Jad5lUvMqveatZ6eP9JnVG/uDlj+FKUkldlRpuTsjW8yjzPeuHvfGjZK2UAA/vy8n8hWBd6zqF9kT3UjKf4Adq/kOK554qC21OuGBm/i0PSrnWLC0yJ7yFCP4d2T+QrIuPGmnREiITTe4XaP1/wrz7NJWEsXN7HVHBU1vqdhL46kJPlWK49XkJ/kKpy+NNSf7kdvGPZSf5muborJ16j6myw9JbI2H8Uas/8Ay9bf91FH9KrvruqP1vZvwOKz6SodST6mipwXQuNql+3W8nP/AG0NRte3TfeuJT9XNV6KnmY+VEhlkb7zsfqaZmkzRRcdhc0UlFIYUUUUAFFFFAD1Qt9O5PQU8Qg/8tU/X/Co9zbQueB0FWrGFJJGlm/1EI3ye/oo9yePzPagcVdkq6TIIlmnmhgiYZVpG5YeoA5P5UFNMhP+suLgj+6ojH5nJ/Sqt1dSXdw80hG5j0HQDsB7CoaC3KK+FF/+1Hh4tIorf/aRcv8A99Hn8qpySvK5eR2dj1ZjkmmUUEube4VIk8sX3JGX6Go6KBJtbHTaLdT/AGSe9mkDGM7IsqMhj3z7f1rPvJ8fvH5ycIp/nVzT0J0S3jHBluGP6KKxr6YS3blfuKdqj2FB6Fao40IxvuQPI0jbmOTTaKKDzmzU0G7S11JBMcQTAxSn0VuM/gcH8K2rWebRtU+YYZG2uPXmuSBxXUbzqOm2twTmXBidvVl6fpj9aaPUwFV2ceq1X6md4i01bDUPMhXFrcjzYfQA9V/A8flWPiuwtQmsaedHuWCSqxa2kb+F/wC6T6HjP0B7Vyc8MlvO8MqFJEYqysMEEdqRzYulyz5o7MjooxQBQchPAu0NOw+VOB7sen+P4VBWhPaTmWKzijZ2VFbagySzAE/0H4UGygtj/plyqsOsUPzt+J6D86DR02UMGlCM33VJ+gzV77dBDxb2cf8AvzfOfy6fpTW1a+PS4dB6J8o/SgXLBbspFSDgjB96SryapP0m23C+ky7v16ilaTTphzDLbt/sHev5Hn9aB8sXsyhikxV9dPWb/j2uYpP9lzsb9eP1pG0nUF62c2PUISD+NAvZy7FGip5bO5hGZYJUHqyEVBQS01uFFFFAgooooAKKKKACiilAJ6UAJRRRQAUUUUAFFFFAC0UlFAEiSFTW9o2uSadLjHmQOfnTPP1Hoa56nKxU1cZWErxlzR0Z7hp3iLT77Ro7a+je5sRnypEx5kJ7j3+lWbS+0LRSbnTknvL0f6lp02JEf72P4iK8b0zVZ7GYPE2VP3kP3WrtLPUYL6DzITgj7yHqp/wrVWep7eHzDnh7OTt+poXFw88ryyuXkdizsepJ6mqxPNNZ6buqjSpUuPzTSaTNNJpmFwY1Cxp7GomNBI0mmE0E0wmgCRJAhIbO1gVbHoaY8bxNhh7g9iPUU0mm5oFcvWjYcGuq068wgjmjSeP+6/UfQ9RXGwSbWFbdlc4xzSZ00J2Z2tltsxc39tlnit2eFXwSjZAz74zXAw6xqcWtC8F1OLoPkSbzk11FjfNBIHTa2QVZWGQynqD7GrMUOg284uvsNw8qncImlGzP1xkj8BUbHq0asY3clf8ArY0vEiBdTSYqFe4t45pFHZ2HP8s/jXI37jmtLVNWkvbmW5nYGRzk4GAPQD2Armr263Z5qtzknPlgk+hBIVLGmYU1Sec7qb9oNOxx+1Re2KaPKXPSqYuqcLrmiwc8TcsYlLCuhhQLGK5awuvmHNdLbTh0HNI7MPKJYpG5FLmmuwVSaZ2tqxh6ogwa5WcYkNdLqc2Qa5mc5c0HjYjcYtWYxVdatwjkVcTim9C5CnSrSjAqGIcVNXTFaHnzldi0UlFUZi0lBNJQMWkopKBAeaglTIqemOMik0VF2ZlTLjNVHFaFwOtUJK5pI76buiKgDNGMnFWoYM4zUHRFXGwW5dhxWvDaiNMkU23RUxU81wqoeaR0wgoq7Kd1KEUjNY8j72Jqe6mLsaq4pmFSd2FFLg0YpmZ1ZtmSm/d61otMjIayLqXDECu/mPlKuF5S3HdKnep/7RIGAawldmNXra3aQjOapSbOR04x3LTXU0pwCau2tpLNyc1JaWSDGa3rRY0AAAocW0aUsTGD0OcvNPaMZxzWWylTg13s9uk6YxWJdaMSSVFRex7FOtGaOcxS1pPpci5yDTI7LL7SeaLmuhWhhaRgAK6nSrPy1DEVHYaaFw1baKI1wKaVzixWIUI2Q48DFNoJpK3SsfOVajkwprHApScVA70zK4MwqN9jjBxUbyVA0tJxudFKq4MHsoWOeKiltkRDt60pmPrTGkyOtRyHc8bJqxiXiNk9azhIUet+6RXBrFngy3FS0OlLnepqWV38oGammuTt61iRM0XWrAmLtildnasJF6krSyMe9TRRO/OKmtIBJgkVqxwIg6Va1ODE01TZRhtCTzWlBbBRT0AHQVOtWedKYqqAKhnkCqfWpnO1SaybqYlutAo6sgmJcmmR2zO1TQL5jVrQ26qASKLXNXPlRVh09SnIofTh6VpDjpTsilyjjiZRMldOUHpVyG0VO1WePSl3UcpU8VKSAIFHFIUpdxo3VRyuTZEY6iaKrWaQgGgEzOeKq0kPtWq6CoHjpWNYyMl4qgZMVpyRVVkjqbG0ZFBhio2qy64qs/FQzRMiZqgZqe5quzUjRCl6TdTCaTNItIk3VDdX1vZQ+bcShF7DufoKyNU1+Kz3RQYlnHH+yv19TXJ3N1NdzGWeQu57muWriFHSO520cI56y0Rtah4puZyUtMwR/wB7+M/4fhWAzM7FmJZjySTyaSkrhnOU3dnpQpxgrRQtFJRUFi0UlFABRRRQAUUUUAFFFFABRRRQAUUUUAFFLSqrOQFUk+gFADaKtppt9J920nb6Rn/CrCaFf43TRC2Tu1wwjH68n8KC1Tk+hQijeWRY41LOxwFAySatXhW3QWUbBghzKw6M/wDgOg/E96lee3sInitH86dxtacDAUdwueefWs2gHaKt1Epc0lFBAUUUooAKKK0dH006leBXby7eMb5pcfcUf17D3oKhBzkox3NeAfZ9OscjlInlOffJH8hXL966TUrlZYruaJNkQURxrnoOAB+Qrm6Dqxlk4xXRBRRSUHGLW1odxujuLE/ekxJEfR1/xBNYtPilaGVZEJDKQQR2NBrQqezmpHRy/vIkvIsBs4kUfwn1qxqNtb65aC/MqQ3kCBbgtnEi9FfgHnoD+BqqJhG0V7GoaGcHzE/9CX/PtU8TnTNQSRcSQuuRnpJGwwQfw4oPZajUVnr/AFozHSHT4ZMyz+cB/CqkA/1qy15ppffsjBHACw9P1qprViNP1KSKMloWAkib1Q8j/D8Kzs0HmOs6bcVFGre61LLG0Fu7RxMMMQNpb8u1ZVJRQc86kpu8haKSiggWijNGaADNSLPMn3ZXH0Y1HRQCbRYjvrqNsrcSj/gZq1LFHqFubi3jC3EYzNGvAI/vKP5jt/LNqSGaS3lWWJ2R1OQynBFBpGfSWqFitpp32xRO7eijNWxo9wP9bJbwe0syg/lnNRS6leTJse4cp/dBwD+VVc0BeC8y62lS8+VLBOQMkQyBjj6dao4xT0kZHDqSGByCOoq7dgXluLxAPNB2zqB37N+P8/rQKyktDOpcUU+OJ5WCorMx6BRk0EDKfgLEPVv5VaFnFAM3c4Q/884/mf8AHsP5+1NkuYTjy7ccDALtn/CgrlstSpikqUy5Odq/TFNbYRlQQe4NBIyiiigAooooAKKKKAClpKKAHhsVctL2SCRXjcqw6EVRpQcGqjJolq53Wnaol6u1sLMOq9j9Kv5rgLedkYEMQQcgiur03VBdKI5SBL2P97/69dEZJnTRxLvyTNXNNJpuaQmqO24MaiY05jUbGgLjSaaTQTTaBAaaaWkpCFBxVqG4KnrVOlBoGnY3Ib8gdanOpHH3q54SEUvnH1osaqs0ak98W71mzTFj1qJpCajJoIlUcgJpKSimZi0UlFAFq2mKEc1uWt/tAya5kEg1Ok5XvSNYVHE69dSGOtNk1AMCM1zAuyO9PjuizdaVjoWIb0Ll7KXBrEc/Ma1JG3LWZKMOaEY1u4J1q7D1qihq7Cea0icVTY0YulS1FEeKkrpWx58txaSijOKoQUZpKKQBRS0lABTX6U6mP0oYLco3Hes6TrWhcHrWfIea55ndS2GxjL1oxcLWdF9+r4+7WLO6lsEtzs4zVSS5L96bct81QDmmRObuO+8aeseaWNc1dihzVqNzCU7FPyjQY8Vpi346Ux7fjpVOBmqqL6FmIpZbYYyetThViGTVaa7DNgGupHj4mouXQakaqelXoXC1RDZ5qZHxWqPFm2zZhmxjmtCKfpzWBHLirsU3vVpnO0dBFcetWBIrCsOOerKXApOKZcK04F64CeU2B2rm3l2XP41ryT5QiudvH2zZrNxsd9LFSkrM6yxmDRD6Vb3VgaVc5QDPatXzh61pFKxwYiblLUtbqaXAqsZqjaf3qzmsWHl461VklqGSf3qs83vQNImeX3qBpaheWojJmlctInMlMabAzUBf3qC4lwp5pNlqI+W6ycZpI0EnOKyzKS1adk/TNZvU7aTUGR3MG3oKrxRtvHFbjRLKBSJZqDnFQepGvHlJLFNoGavbuagXEa4FKGya0ijysXVUi0hzVhKqxmpi4Rc1oeaxtzLhcZrHlJd6s3MxY4FRwxF2pGkdEWrGLpWoBgVBbx7FFTimjKTuxaKKKZAUlLR2oAKKSjNIYtGaaTSZoGOpjAGjNGaBoryJVSVKvsKrSr1pGsWZcq4qjKK05x1rOmHWoZ0QZSkquxqeWq7VDN4jCa5nWddLbra0f5ejyjv7D296XX9XILWVu/tKw/kP61zea4MRX+zE9TC4ay55ik5pKSiuI9AKKKKACiiigAooooAKKKKACiiigAooooAKKKKAClopQCaAErWa6n07TLeGCVopZsysUO0hegGevYn8RUdpZiCNry9ibykOFjbjzG6gfT1qlc3El1O80pyzHnAwB7AdhQaq8Ffqx7X94/3rqY/WQ1A7u5y7Fj6k5ptFBm5N7sKKKKBBRRRQAUtFFAEttbS3dzHBCpeRzhQK6G5eKyg/s+1YNEhzJIP+Wr+v09B/iaj0uBtO01711xPcrsg9QnRm/Hp+dUrif7MueszDKj+6PX6+n5+lB6FKKo0+d7v8hNRnVLZbReX3b5OOh7D9ay6CxJyeSaKRxVJucrsSiiimQLRRRQBraPMJA9i54m/1ZPZ+359PyrQt91xZPA337YllB67T1H4H+dc0rFTkcV0tld+bcwX/AFLHy519yMZ/Ec/XNB6WDq3ag+n5f8Aj1dRc6FbzHBktpDFnuVbkfkQfzrna7S2077Y95pwcKHyAW7d1P5j8jXM6jpN5pkuy5hKg/dccq30PSgWOoyUuexQooooPOCiiigAooooAWigCnhaBpXG4o21MEp3l+1BoqVyDbSYqwY6YUoB07ENS29y9vJvTHIwykZDD0IphWm0GeqZeF3Zj5jp6lvQytt/Lr+tRy380ilECQxnqkS7Qfr3P41VooKc5BRSUUEC0lFFABRRRQAUUUUAFFFFABRRRQAUtJRQA4HFWrecqw5wRVSlU4NVGVmTKN0dppt/9qj2SEeavf+8KvE1xtncNG6srEEGupt7gXEKyDr0Yehrqi7o3w9d/w5bkxNRk0pNNJoO0Q02lpKACkNLSYoEJRS4ptAC000tIaAENNNKabnNAgzRSUUAOoptFADqM0maKAuLmnxth6jpV+8KBpmgDlKpXH3quRglKq3KHNJG1TWJCpq1C/IqlnFTRvg1aOSWxswvkCrGeKzYJelXkfIroizhqRsx+aKKKsyCikooC4tJRRQIWopGwKezYFVJpODUtmkFdladutUJDzU8z5qq5rnkdsFZEkH36vj7lZ9v9+tD+Cs2dtLYz7j79Rr1p05+emqeaZjLcuW65NakS4FZtsea1Iz8tbU0cdZklIQCOaKXtWpzXK887sOtUdx3c1bIyMVVkXBrRo8JTb3LUL5FWQazIpNpq9G4YVSZlOJaV6mSXFUwaeGqkzJxNJJ/erC3HvWQJMVIJvequRymsJ8jrWPqDYapRP71WvG3rmpkzWkrMtaVdYOM1u/aOOtcZaTGOXrW9HcbkHNEJBWp3dzUNx71E1x71Rab3qNpveruc/IXGm96haX3qqZfemGSlcpRLBkppeq++k3+9K5SiWC9VLmTNPL8VSmfLUmy4x1BeWrStztWs2LrVxHwKEORpJORUwuTWar1Kr09COaSL4mJ71Kj1QV6lE4XvVIzd2asbADJqKe444NUftnbNNDmQ0XFyWJly7Vp2kOACRVW1gJIJFasabRimkROQ8DFOpKKZiLRSUUALSUtJQAU2lNJQNBSGlpDSGJSZoNJQMDUEnSpiahfpQUihOOtZs4rVmHFZs461DOiDM6QVga/qf2CDy4j+/kHy/wCyPWty+njtLeSeU4RBk15pe3cl7dyXEh+Zz09B2FcWJq8istz1cFR53zPZFcnJzSUUV5h7IUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAUU5VLdATT8KnXDN6dhQBHilAp4lI/gQj0K1bs5oluVl+zRkJ8zBiSMDnpQNK7FW2gs4EmuwXlcZSAHHHqx7D26n24yq3ts33rYRN2eEkY/A/wCNUZpnnlaWRizuckmmUi/aW+EtXd155RFZjGmdu7qSepP6fkKq0lFMhtt3YUUUUCCiiigAopaVVLHAFAABXRaTpNvb2y6jqahlbmC2zgyf7Tei5/E1HpmjiFlu9UiZYQNyQnhpT2+g96L3UDc3E08mMoM7QOB2C+w/wpnfRoRpx9rV+SHajqPJkkCmQ/cjC4UDtwOgHYVz8kjSSM7sWZjkk0skjSuXc5Y9TTKRzV6zqyuwooooMQooooAKWkpaACtDR5dt8sRPyTfIfqen64rPp8TmOVXHVSCKC6c+Sakuh2FqxlvZAMhpYGHH94D/ABFV4NYuIMqWEiHhkkG4H61ZtSsevQf3WkBH0OD/AFrnLi7lt7uaEhDscryvoad7HvYivGlFN9Tfe20TVBh4DZTH/lpDyufdTx+WKwdU0W50twXAkgf/AFcyfdb/AAPseadHqMRxvjKH1Q5/Q1t2OqqITFMqXNq/Do/Q/wCB9KNzllHD4le7pL+tzkKStzVdC8hDeWLNPZHqf4o/Zh/XoaxSKR5lSlKnLlkJRRRQZj1FTImaYgq3EmaZ00YXFSLNSiA11vg3wa/iSWae4n+y6bbYM9wRnk9EUd2P6flntt3g7Rj9ntdAguscGa7JlZvfrgfgKpRbPWoYSVTSEbnjjQHHSoXiPpXtTaB4T8To0cMK6XdkfLJb5Kf8CQnp9CK838S+HL7w3qT2V8gDY3RyKcrIp6Mp9KTVjOthnB8slZnKSR7T1zULDFXZUxVRxUnl1oWZHSUGigwCiiigAooooAKKKKACiiigAooooAKKKKACiiigBaKSloAkjfBFbemXvlNgnKngisEGrNvLtbrWtOVmZVI9VudiTzTc1VsZ/PtcfxR/yqxmuhnoUKvtIJ9RaKTNLSNgooooADTTTqaaAEpppxpuM0CG9aTFShM04R07EuRBikIqz5VIYjRYnmRXxRUrR1GVxQO4lFIeKTNIdx1PiXc4qMZJwKuWkWWBNIqKuzYsrPzEHFF7p21M4rU04KsY6VNd7GjI4pHpKknA4WeIxuRUQbFa9/AGY4rIeNkPSqTPNqQaZYikxV+Kb3rHVsGrCS471pGRzTjc2kkBqTINZcc/vVlbj3rVSOWUC3RUAnFL5w9armI5WTU1nAFQGYetQvPx1pORSgyWSYetUZpc96bJNnvVV3zWTkdEIWB3qEnNDNT4kLtWZ0JElshLDFaflNsp9hZFiOK3U07MfSpZ20qbaONuIWDmq+CprqbvTSMnFYtzaFM8UJmVSk0RQPg1pwyjFYoJQ1Zjnx3rWMrHFUjc2A49aGkAHWs4XPvTWufetHMwVPUuVFMOM0u8AVHJJkV0NnzUU7lUthqsQzVAU3GnrERUo2laxfWXIqQODVAZFPEhFVcxcUXd1G+qolpwcGncjlLPmGmSyZQ1FuprnK0NlQjqV95WTNa1pcAqATWK4O6pI5WSoudypp7nRghh1pki4GazILwkgZrQEgdKpMVWhFRuiFnwabvpkjfNTN1O5wcpNvo31Duo3UxWJS3FVJW+apt1VpqTLiiWJ+atq1ZSPhquxSZFCYpxLitUyNVRWqZWqjKxK820VVa5OetLOTiqqKWek2XFIvwMzmtuygJxkVn2UIwM1u2wCgVcUYVJF6GIIoqWmocinVZyN3FooooEFFFGRQAUlGaTNAxaSjNJmgYUhpaSgY00hpaSkMQ1G/SpDUbUDRUlFZ8y1pyisu/nS0tJrmT7kSFz747VMtFdm9NNuyOB8ZajunWwjPCfNJj17D/PrXJ1NdXD3d1LcSnLyMWY+5qGvCqzc5OR9XRpqnBRQlFFFZmoUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAoopKKAJEj3DJZVHqTTy6pGyRkktwWIxx6VDk4A9KKACkoooAKKKKACiilFABRShSTgVrW+mQwMn252Mz42Wsf3znpuP8P8/pQXCm5vQj07SvtURurhjHaIdpYDl2/ur7+p7fkDqrqcNguLKCK1H98DLn/gR5/LFVtW1DynFrEFCxDYir91R/U5yaw3kZ2LMxJPc0HW6kcP7sNZdWaV3q8k2djsWPVz1/CqjEpYDP3pXz+A/+uT+VRwQ+dJgsFRRlmPYUXMyyyAINsajagPp/jQc86sqnvTZBRRRQYhRRRQAUUUUAFFFFAC0d6KKAOmjlPl6dcjrsH/jpx/SsvX4vJ169XsZSw+h5/rV+L/kFaeT/ALf/AKFVfxQuNadv70cbf+Oig9bFe9hk/T8jGzUkUzwvuRsH9DUVFB5SbWxv6fqrq48qQxTdNu7hvp/ga1IbvTbt/L1HTYXzwXQeW4Prkd/rmuNzitO2u/PURSnEo+4/r7H/ABp3PQoYu9oVFdGnrXhVrWE3umSG7sep/wCekX+8PT3H44rmsYNdZYavPaEBWIx1FaF1d6bHGlzLYWIaTlXkiyWx1OB1+pFFjoq4CnNc9OVl2ZyVlY3V6222t5ZSOuxScfX0res/DziVRe3lraLnnc/mMPwTP6kUlxrKzjYb4iIcLHFFtUfQDAqOO7tsYE8n/fr/AOvQOjRpQeruel3OsaRbeHbTRdLv1WGJcu/ltl3PVjx1P6cVy04aKUqzBsjIYdGB71qv4TjttOs9QOomWzuohJHKkXB9R14IORWZeMjzKsIbyo1CLu5Jx3q9bH0uCdqdorQW1neOZWViCDwQeldl4pgTX/he97KAbvS5FZH77GIDL9OQfwrireJ5JVVRyTxXa6640f4W3qTHEl/IkMSnqeQxP5Kf0oWq1M80UXRTe9zxOYVRkFXpz1qjIeazZ8libXIT1pKD1ooOEKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigBaehwaZQODQhM29MufKmUnlTwR6itthhiM5HY+orlbd9rCumt5POtVfuh2n6dR/WuuDuiKE/Z1eXoyQU+mCn0z1QpKWkoAKQ0tIetAhuKeqZoVc1aiiz2qkjKc7DEhzVhYPap44gBUwUCtlA5JVSp5FIbf2q7ijAquQj2rMx4Paq0kWO1bTRgio/sRkPArOUTanUbdjBZD6U0ISa3n0w46VTktxETxWTO6NN2uyrHFjkirCOIzmo2cKKqyT5PFSW5KJsJqZjGA1K2qlhgtXPlz60m8+tOwvbyNtrgS96hkjDis1JmU9auxThhyaRSmpblaWEocjpUW7FabKHWqM8JU57U0zKpTtqhqyYqUTVUzil3VVzBxLwnpftHvVHfRvp8xPIi4Z/eommqAvTS1K41FEjPmoi2aTNOVCxpXLSG9a0tPh3OOKrx21bWnwhWFS2dFKm76m/p1oAgJFamwAYqGzAEQqwaR7dGCUSCWBZFPFc7qVqFzxXUVh6sRzTMsTCPLc426TaxqqHxV29PzGs49aZ4c9ybzfekMnvUVFO5FjU8wmlALGhUzU8aAV2o+UbsOij45qcRj0pFp4q0jCUmRtEKgaPFXD0qNhmhoFIpkEUm8ip3SoGSpNU7jvNNIZs1EVNNINI0ilcsJhmqZoAVyOtU0faasifikdakrEe0xtVqO6wuCaqSSZqDec0J2InK6NLzNxzTs1ThfOKs5q0cMlZj80ZpM0UyR2ajkGRTqQ9KARUIwasQmoZOtSw1KNJbFtTUymoFqRTirMGPkORUcQG+mSSU6A5YUD2Rt2vAFasDdKx7c4ArTgbpWiOWZqxHipM1WibipC9Uc/Uk3Uheoi9ML0DsT76QvVffSb6B2LG+jfVffRvoHYsb6XfVffQGoCxZDUuM1EhzSyTLGOTUN2OmlQcyQimkVXF4pOM1OsgccUlI0qYWUVcTFNIqQ00irRx7MrSCuH+IF/8AZ9MislPz3D5b/dX/AOvj8q7qQcV4941v/tviS4VWzHb4hX8Ov65rkxk+WnbuelltLnrX6I52koorxz6UKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigAqWCCS4mSKJC7scBR3piqWYKoJJOABWlMy6ZC1tGc3bjEzj/lmP7g9/U/h60FRjfV7AbiLTQ0Vrte46Ncddvsn/wAV19MUaKd2qCZ8t5aPIT7hSf51mVfsCY7e8mH8MWz/AL6IH8s0I1pyvNdkU5HaSRnY5JOSaZRRQYt3ZZJK6cuDw8pyPXAH+NVasXDbUjh/uZJ+p6/0/Kq9ASYUUUUCCiiigAooooAKKKKAFoooHWgDoVGNO01f9hj+bn/Cq/ifjV8dxFGD/wB8irYH+j6aP+mI/wDQmqn4oP8AxP7gDsFH/jooPXxKthfu/IxqKKKDyBaAcGkpaANS2m85OT+8Xr7j1rU1G1+3aElzGMzWQCyDPJjJ4P4E/rXMpI0bBlOCK6bQNWhW52SqfnBR0xlXUjBH5Zpno4apCpF0puzexzqGrUTUzULb7FqE9uDlUb5G9VPIP5YqNHxQjCEnCVmek+CvGdrp1lJoeuQvcaRK+9WTl7Zz1ZfUHuPxHv2aeDLHVALjRdUtbqBuVxKMj2I6g14YkuKmW5I6HFUpNHq4fGTpfAz2t9K0jwr/AKRreoQIV5WCJg8r+wUfzPFeceL/ABZceJdRErIILSEFLW3B4jX1Pqx7n/CueS4QnEhYKf4hyR/jUE5KHqCD0YdCPahyuLEYudXWbIZnyTVVzT3fNQk1B49WfMxtFFFBiFFFFABRRRQAUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAUtJS0ATRNg10GkTZbyieHG38e361zanBrUsZdsinPSt6MrM5660ujoB79aUGlmOX3jo43f4/rmo81s1ZnqU6nPFS7kmaKZmjNIu4+k703NOXrQhNk8S5NaEUfAqpAORWigwK6II4q0hw4FFFFanKFFFFACir9tswM1n05ZCvSk1c1pT5Xc1J2QRnpXM6hKAxxV24uW24zWJdOWJrmlGx6axHNGyKkkhY1FmlamZqSL3FopuaSkIdmnJIVNR0maAvY1IJ9wwasMgkWsaNyrcVpwXAIGaTR0U530ZVmt2VjgVD5TelaxZWpNimi4OkmZXlN6UeW3pWr5amlWBWai4vYmYsDN2NSfY3x0NdJZ6argcVojSU29KLmscK2jihaNnkVYjgCit67sliB4rDuZhGSBQJ01T3H7lWrFrdAP1rEknJPBoinKnrzRYj2tnod9Y3q7Rk1oi4QjOa4W11ApjmtFdU4+9TO6lirI6Wa6RVPNc5qV2GJ5qCbUiwPzVk3N1vzzSMq+I5ivdPuJqnT5H3Go6Z5zd2LmjNJRQI2VNTK1VVaplNdyPk5IsqakBqFDUy1aMWONRtTz0pjUyURtUZqRqjNSzRDSBSEDFOpp6Ui0yuetSIM1G3WpYulJGjbsOKVDImDVqo5FyKGiYyZFE2DVxWBFUCNpqSOQihMco3L1FRpIGqQVRi1YWkPelpKZJWk61LD1qGT71SwUupo9i0KczYWmio5W4xVGSWpEzZar1ovQ1RjUs1asCbVFCCo7IvQ8YrQhNZ8VXou1aI5JGhG3FKXqFWwKQtVGdiUvSF6hL0m+gdiUtRuqHdRuoAm3Ubqi3UZoCxNupQ1QbqUNSGkXEbisrUbkgnBq6JQq8msu+XzDxWMtz3MClbUppdtv61t2NwXUZrAW2fdW1ZRlFGalHXiUuU1w2RSZqLfxRvrdbHzdRe8RX1ytpZT3LcLFGzn8BXgc0jTTPI5yzsWJ9zXrvjm8+zeFrlQcNMViH4nJ/QGvHzXl46V5KJ7uUwtTcu7ENFFFcJ6wUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAUoFFaEFtFb263V4CQ3MUIODJ7n0X+fb1AVGPMV7exubvPkQs4HUgcD6noKsDSWUZlu7OPHXMwY/kuahudQnusK77Yh92JOEX6Cq2aB3gulzRFzbaeG+xky3B4E7LgJ/uj19z+VZpJJyTk0UUCcrhWhtMGjEng3EowPVVHX8z+lQWFt9ru0jZgifedj0VRyT+VLf3QubjKDbEg2Rr6KKCo+7Fy+RVqRMIvmHk/wj+tR1JKfkj/3cfqaDMiJycmiiigAooooAKKKKACiiigAooooAWgdaKB1oA6i2QSDTFP/ADxGf++mrH1uTztWnl5w5Dc+4Fbijyo7M91st34nJ/rWHqqENbv/AH4s/kSP6UI9fFr/AGdL0/IzqKKKDyAooooAWpIJDDOkg/hINRUuaBp2dzd1uJZbW2u1HP8Aq2/mp/n+VYoOK3NOlS8sHtJmADALuP8AAR91v6fnWRd2stncNDMm11/Ij1B7ihnXildqrHZ/mNElOEnvVfNLmg51UaJ/MpyTAZR+UP6H1FVs0ZoD2jJZkEbEbsnPIxjFQ1NOd4WYfxcN7GoaCHuJRRRQIKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigApRSUUAOFW7ZsMKp1PAcEVcHZkTV0dZE2+wifurFT9DyP5GkzUemtvsp4x1C7h+B/wzS5rsl3LwUrwcX0ZJmjNMzRmpO24/NSIeag3VIhoQmaNv2q+vSs23bpWih+WuiBwVdx9FJmitTEWkoopAFJmlpDQBXuDwax5+prVuW4NZE55NYzOqiVmqOnsajJrE6QpM0UlILi0lJmimAtSLIVqKlzQFy0tywpwuzVSlpFKbLgu6sW92N4zWXTkbac0WKVVpneaZcoQOa1zIuzOa4OyvzGRzW0mpFo8ZpHpUcR7th2q3I2tg1yN1Juc1qajcls81iuctmmjir1OaQ2koopnOPWQrUguGHeoKKQXZM07HvUbOWptFANiUlKaSmIKKKKANNamSoFqdK7EfKyLCVMtQJUy1ojnkP7Uw1JTSKZBERUZqYioyKTNEyPFNPSpCKaRUlplV+tPiNEi0xTg0jXdFsUU1TkU6mZPQjaPNRGMg1ao2g0WGpFZWIqxHLng1G8XcVGMqaRWki+OaUIT0FR2zbiAa2IrcFRVXCNFtmJJCc1Yt4TWhJbqO1JGFSkdf1bQrtEVFUpMlsVrybWWqgt9z0zJ4flVyK3i5BrRjGMUJb7VFSovNaRPPq3TJoh0q7HxVWMdKtp0q0crJs8U0tSE00mmSLmkzTc0ZoGOzRmm5ozQMfmjNMzRmkA/NMeQKuaRmCjNUJ58k80my4xuySS6OcA1JD+8PNUEUu2a0YRsFQ1c7Kdbk2LSQqOtTBgo4qr5p9aPMoUbDqYqUlYs+ZS+ZVTfRvqziauzkPiNdZt7G2B+8zSEfTAH9a8+rqfHlx5uvLFniKFR+J5/rXK14mJleqz6fBQ5aEUFFFFYHWFFFFABRRRQAUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAUoFKFJOAOafHIY1cLjJx83pg9qAJVCWy7nAaY/dQ9F9z/h+fpSXjvI6M7FmKAkk9arnJOetS3P+sUdwij9KCr6WIqKKKCQooqzZ24mkLyErBGN0jD09B7npQNK7sWFItNJYYxNdHHPaMf4n+VZ1TXVwbicuRtXoqjooHQVDQVN3dl0Chm3H09qKSggKKKKACiiigAooooAKKKKACiiigBasWUAuLtEb7g+Zz6KOT+lV6uwEQ6dPL/FIwiH06n+QoLgk5amu9wZbO0m6fumj+mCcD8iKh1e03aVb3KDIV2RvYHBH67qhsnMumTRdTC4cfQ8H9cVq6ZIstnJBMvmRg4dc9VP9cjNHQ9eP+0Q5erX4o5KkrT1bSJdNkVv9ZbycxygcH2Pofas2g8ecJQlyyWolFFFBIUtJRQBLBM8EgdDgj9a3LgpqOkueS0C+ZGx6gZwy/1/D3rn61tIJeG5iHJMbYH1B/qBQjpw8m703szJopT1pKDmCikooAkjYAlWJCN1/wAaUxD/AJ6xn8TUVLmgAYYOMg/SkoooAKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigAooooAWpIjg1HT0PNNCZ0ugvm6WMnh/kP48VY2npjmszS5DHMjDqDmugmhxcy46bzj6ZrtjrExw0uWpKJS20hFWzCfSmNFinY71NFXmnqaVkxUecGpKvcvQPitOJ8isSN8Vehmx3rWErHPVjc06KijkBHWpQa3TORqwtJS0mQKBBTHYAUM4AqnNP71Ldi4xuRXEvWs2VuTU00uaqO2TWEmddNWGMaZSk02oNQpKU0lABRRRg0AFFLtoxQAUA0lFADqWkBpaBkiMQa07eQlKylrSslLCkzai9SK8yRWeetbF1Cdh4rKdCDQgqq0iOilIpKDEKKKKACiimmgBTSUUtABSUtFMDRWpkqBamSuxHy0iylTLUCVOtWjnkSCgilFLirMiMioyKsFaYVpWGmQFaaVqcrTStKxaZXZeKqSHaauy8Cs+U5NRI6aSuSRy+9WVcEVnqDU6sRSTKnFFylFVRKakE1VcxcGT4zSeRvPApqyg1ftdrYNMqEXcihtyh6VfWfYmM06TaEqqetI9WlBJD3lLUzJpKKDUduNSRvhhmoqKBNXNSPDLTtoU1Rgn28GiW6JPFWmeXiqHU0lZV71J56KOtYgnY08SOavmPNdM1GvFFQtfD1qgyOageNxRdjjCJrx3YY9atBgRkVz0RdW71r20uVANEWTOCWxbozSZ4pCwFUY2HZqGScIOtRy3AAwDWZczk5wals2pwu9S1LeZ4zUSt5jVlGVi1aFo2SKhO50yppLQ0oUCjNS7qjB4pdwqzldyTNJupmaTNMRJvo31ETSBvmGemaVxpXPMvE03n+I7585Ak2j8OP6VkVYvZTNfTyk5LyM35mq9eBN3k2fW048sEgoooqSwooooAKKKKACiiigAooooAKKKKACiiigAooooAKKKKAHmQ42r8o74700UlLQBIBEOSzH/ZA/rTXYu5Y9SabRQAUUVZjhRIxNPkKfuoOr/4D3oGlcbb2sty22JCx7+g+pqe+YW6CxjIIQ5lYfxP/AIDoPxPenW1w0twoY7YYwX2KMDgZqgzFmLHqTk0FtxUbLcbRRRQZhRRRQAUUUUAFFFFABRRRQAUUUUAFFFFAC1bl+XT4F/vMzfyH9KqCrt0jJYWJOMMjEf8AfR/woLjs2TaGd180J6SxOmPfaSP1Aq9p7lftKjqYH/Tn+lZ2iNjWrP3lUfnxWppQH9pqOx3A/TBoR34R+6vUnsL2Mg21wiyW8nDI3T/631rK1zRjpc6vGWe1mG6Jz19wfcUsbLMheHIK43Ln7vuPat7TbmDVbOTTLsgBx8pP8LDow9x/KnubuMcTDlfxdH+hxVFX9S0ubTpmV+VDFc+hHUH3/nVCkeROLg7S3EpaKKCQq7pl0LS7WQ4weOeg5qlRQVCbhJSXQ3bjSEuvntNscrc+VvBVv91v6H8zWLLE8MjRyIyOpwVYYIqW3u3gOByh6qa15JrXWYEjkkEV0nEbydx/dJ/kfw+gdElTqq8dH2MCkrSfQ9QRiBBvx/zzYN/I1Tntp7Zgs8MkZPZ1IoOeUJR3RDRRRQSFFFFABRRRQAUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAUUUUAFFFFAC05etNpV60Aati2JFrtBGG2N/eRT+n/1q4eyPzrXc2zbrS3P+xj9TXoYfVHDJ8tYd5QxUMsIx0q1SNyDW7ijdSaZkSx4qo4wa0rgVnSda55I7ISuNDYqZJcVWpQ1JM0auaUdxjvVlLn3rHWTFSLN71amYyppmx9oHrSNcD1rK8/3pDOfWq5yPZF6W496pSzZqFpc96hZ81DkaRgkOd81ETQWphNQaIWm0UUDCilpM0CFAyalVM1GlXIlzTSJbsR+VxUbJitIRjbVaZMVTiQp3KJGKSnv1plQapiipUjLGmxrk1rWVrvI4pGkI8zIYLJnxxW1p+nMCMrxWlY6eNoyK1o7ZIxwKTPSo4bqYtxp25OlY0+lkEnFduY1IwarzWauOlBrVw1zz2ezKdqpsm01219pw2niuZvLUox4pnnVaLiZhpKe4waZQcwlFFFABRRRQAUUUUAaC1MlQA1KprsR8xItIanU1VQ1YQ1ojnkiwtPFRqalFWjBihaQpUiinhadiblcx0xo6u+XSGKiwKZkXCmqJjLNW1cQ8ZxVNYsNWbiddOpZEcdt8o4pxt/ar8cY2DilMdPlIdZ3M02xqMwEdq1ClMKUco1VZmiNh61ctt46VMIxnpV23gUjpStY3pVLyIC77cGkqzcRhRwKrUj147BRRRQMKKKKAHIpJwKnFoW5psAy4rSH3apHDjJWiUks6uRWqilWrCVqkeHKbG+QoHSontlYdKtHpTKdjNSZnPa4PSo8mPpWk+MVQnAOcUrGsZXE+1kcUx7lm71F5RJqVLcmlqVoRZZvWkNuXq8sAWpAoFFg57GQ1njnFPiUxmtJkB7VWePBpcti/aNoTzSe9Pjck1FtqSNe9BDsWQeKQmjtTSaZAE4qCaTZFI/91GP5CnO1Z+py+Xpd23pC38sVE3aLNqUbzSPM2OSTSUppK8E+rCiiigAooooAKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigBamit5JgWVflHVicAfjTIYzLMkYOCxAzUt1ceY/loT5Efyxr6D1+p60hq27HD7Nb8sfOkHQLwg+p6n/PNQSyvM5dzkmmUUwbHocKxwcYxxUdO3HGM8elNoEFFFFABRRRQAUUUUAFFFFABRRRQAUUUUAFLRT4o2lkWNAWZjgAdzQBPZWv2iQlzthQbpG9B/jTbucTzZRdsajai+gqa8lEMYsoj8iHMhH8T/AOAqjQaSfKuVF/RRu1uyH/TdP51pWTbJZ5f+ecUjf+OkD+dUdBGNWikPSJXk/wC+VJqwreXpt7J6oEH4sP8AChHXh9KTfr+Rm2Vx9nu45CMrnDD1U9RWlOptLzzI2yNx59wcEf59axR1ra3Cd9vXzoxIv++Bz/I0GeHno0aOoStNYLqMarIDiO5jYZB/ut/T8PesI/YJjystu3+z86/4/wA62NGu0hd4rhd9tKuyRPUGsfVrE6bqMtsW3KMMj/3kPIP5U2b4q7iqqWj39RP7PV/9Rd28noC2w/8Aj2Khnsri2GZYmVezYyD+PSoM1NBeT25PlyEKeqnkH6ikcN4vpYgoq8HtbniRPs7no6D5fxH+H5VBcWsluQWwUb7rqcq30NBLj1RBRmiigkmW7nUACV8DoCc1Zi1i6RSkhSeI9Y5Vyp/wPuKoUUFqpNbM1l/si8G0rLZSno2fMj/HuP1qjd2c1nKElA+YblZTlWHqD3qAHFaMNwjW8drcf6lhkNjJjOeo/qKCrqe+5mUVblsJ0b5EMqH7rxjcD+VR/ZmU/vGWP2Y8/lQQ4tbkFFSMiqBiRW9gDxSNGQAeoPcUEjKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigAFOHWkFKOtAF60PzCu3sTmxhP1H61w1seRXaWD40+L/eYfyrvw2xwVv4sS/mkY4FR+YMVFJMMV0tm6i2QXDVnSHmrM0mc1Tc81zyZ2U1ZDDSZoNJUGo7NG6m0UAP3Uham0hNAhS1NJoNNNABmkopM0ALRmkooAKKKSgRIpq1C+DVMGpFfFNMTVzUEo21WmfNQ+bxTHfNU5GcY2YxzzTO9KTmkHWoNUW7ZNzCuq0q2BwcVzVkMuK7bSIxsBpM78JDmkacUYRR61JRRSPbSSVgoopKYyKaISKa5fVLXaTxXWVi6sgKk0HJiaa5bnD3KbWNVav3ow5qhQeHPRhRSUUEi0UUUAFLSUUAXgakU1CDTwa60fNNFlGqdGqorVMjVaZjKJdRqnQ1SRqsxtWiZzyRbQVOq1BGatx1ojnloKEpfL9qlUCn8VVjO5RuIvkrLK4krbuQNlZDj95USRvTehbhTMdK0dSWw/d1Iy00tCHLUpslRFcVcZagcUmilIhxVu2YA4qqaVZNhzmpextTlaRfnTcmRWewIOKmN2CMZoC+YMgVme9RmnEr0VI0TDtTNp9KZrcKBShGPQUpRlGSKQm0i3bJ3q2SAMVlJdbDVqO5D96uJ5WMndaFtTUytiqysPWgzhehrU8jlbLm4Ux5FA61Ra4J71G0pNFxqBYkmz0qL7xqIHNWok4zUlPQEiFTAYooqrEXA0w0402gBKay5p1FIaZH5YpcAU+mmixVxCajZqVjUDvUspIR3rK1yTbo12f9jH6irzvWRr740a499o/Wsqr9xnVh43qR9ThzSUppK8Q+lCiiigAooooAKKKKACiiigAooooAKKKKACiiigAooooAKKKeE4BLAZ6ZoAZRUhjcDOMj1HNJtK/e4oAkjzEjS8g4Kr/X9P51DTncuRnoBgD0FMoAKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigBau2R8iCe7/iQbE/3m7/lmqQq7cfubG3h/ifMrfjwP0GfxoLhpqUqKKUDJoINXSUKWt5c9PkES/Vj/AIA069PlaOq5/wBbNnHso/8AsqsSR/ZbOCzx84/eS/7zdvwGP1qjrMgFxHbA/wCoXa3+8eT/AIfhTPRmvZ0OUzavWsjSRrEpxLG26I+p9P61RpVYowYEgg5BFI4Iy5WbCSqxEycK3DKP4TWtPY/2/pqiEg31svyL0Middv1Hb649K59i+8XEPV13Mg/Xj0qzaX+yVJIGaKZTnGf5U7no060XF06mzMgqVJDDBHBBpK6rVbaDWrSTUrcCO9jG64iHSQd3HofUfjXKmkcVai6UrdAqe3uTFlGUPE33kPQ/4H3qCigyTa2Lr2JmHmWe6VD1Tq6/Uf1/l0qo8bxth1Kn0IxSBipyCQauRX8j4iupHlgPBDndt9xnoRQV7r8ilRT5omhmeNuqnFMoIegVJ/yyQ56ZH+fzqOnB8IV6g0DRNK7lC6MQjn51BwA30qvUkMgR/mBKNww9qYw2sQDkdqAbuJQGZc4JGaSigQUUUUAFFFFABRRRQAUUUUAFFFFABRRRQAUUUUAFFFFACilHWm04daALdt1FdXA5TTYj/wBNCP0rlLfqK6ZTjS4/+un9K7KGzOOov30PUsefxUTzZ71W3mml81fMeioIe75qInNBNNzSLWgUUlFIdwpaSigQUhpaQ0AIaaadTTQAlFFFAgooozQAUUmaKQC0ZoopgLmjNJRQAUo60lKKAL9k2HH1rt9IkBRRXA277WFdTpN1gjmkztws+WR1hopsTiRBzTyMUj3YyTVxtFBopjErF1dxtNa00qxoa5fVLrcSM0jjxNRKNjnr1suaz6tXL5JqrTPDm7sKKKKCQpaSigBaKSigC4KcKbSiupHzpIpqVWqAGnqapGbRbRqsxtVFGqzG1aIwmjRiariNxWdG1WVkrVM45xLwenb6qCSgy8VVzPlJLmQbKzM5kqWeYnioY8l6l6m8Y2Rq2w/d1IaZAMJUhq0c8tyFxVd6sydKqyEDNSy4kLnAqlPNzxUlxNjIBqmAZH4rOTOynG2pLCzM4rbtgAgrNgh244q6rEUKJo67jsXNqmk8pagEpFPEtPlLWMZMI1HamSoChFN833pN2aOUznipMy7iNlJxUKTMhrVljDisy5g25IpNWFGfPuWVvuOtOWfeeKxtxDYrRs8nFClcU6SSuaCIzCpDCfSp4cBRUtaJHI3qVY4iDyKsgYFGKWnYhsWkopaZIhpMU6gCgLjcUYqTFGBQO5ERUbGpW4qB2qWXEic1WkapZG4qo7c1LNooazVkeID/AMSiT3Zf51qMayfEB/4lLf76/wBawrfAzswy/exOPNJSmkrxj6AKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigAooooAejFG3A4I6U0knknmkooAKKKKACiiigAooooAKKKKACiiigAooooAKKKKACiiigAopaKAJbaHz7mOLOAzAE+g9addzCe6dwMLnCj0UcAflTrRxF5smTuEZC/U8fyJqsaCm7RsFaOiQJNqSNL/qoQZX46hecficCs2tjRCEhv5Mc+RsH4sKDTDx5qiTLazYea+m+Yx5kwe7E8D86552Z3Z2JLMcknua1tUfybOG3H3pP3r/AE6KP5n8ayKDXFzvPl7BRRRQchamIS3tipIYqTkduT/hUTS7xkjEgOdw7/WluH3yYH3VAUfQVFQXJ66HQeHZy98kTHiQFGHqDwf51gOpV2UjBBwRVzTLg214knpz/n8qm1+28jVpXQfup/30Zx1Vuf55H4UG83z0IvsZdFFFByhRRRQBZlPnWyS/xp8jH2x8v8iPwFVqmgkCEhhlGGGHqP8AGmyx+W+AcqeVb1FBT11I6SlooJEp7EFFOeRwRTKKACiiloASiiigAooooAKKKKACiiigAooooAKKKKACiiigAooooAKUdaKKALdv1FdL/wAwmI/9Nf6VzVv1FdLgjR4v+uv/ALLXXR+FnJP+ND1KxpM0E0mao9MWkozSZoELSUmaM0ALRSZopAFFFITTADShc0qjNTpHmgZBsppWr3k8VE8WKdhFQ0lSOuKjpAFFLSUALRRRQAUUUUAFFFOUZNADkzmtrT3ZCDWbbw7jnFaajykpM6aMWtTpbTUAijJrRS9jcda4M3xVsA1ai1MgctSO2GJ5dDtPtCetQy3qIDg1zI1Lj71Qy6gSPvUzSWL0NK/1IkEA1zl1clyeabcXRbPNUHkJPWmedWrOTEkbcaZRmig5gooopAFFJRQMdRSZopiP/9k=” alt=”testosterone and prostate cancer” data-id=”163315666″ />
How Testosterone Affects Cancer Growth
Testosterone attaches to receptors on cancer cells. This makes them grow and divide more. High levels of testosterone speed up cancer growth.
The Hormonal Connection in Treatment
Knowing how hormones work is vital for treatment. Androgen deprivation therapy lowers testosterone. This cuts off the fuel cancer cells need to grow.
Why Hormone Therapy Matters
Hormone therapy is crucial for hormone-sensitive prostate cancer. It lowers testosterone. This helps slow down cancer growth and improves patient results.
Removing Testicles for Prostate Cancer: The Medical Perspective
Bilateral orchiectomy is a surgery for prostate cancer. It lowers testosterone, slowing cancer growth.
This treatment has been used for decades in advanced prostate cancer. It’s still an option for those wanting permanent hormone control.
Surgical androgen deprivation quickly lowers hormone levels. This is key in fast-growing cancers where time matters.
But, orchiectomy has downsides. It can cause hot flashes, lower sex drive, and mood changes. These can impact a person’s life quality.
Doctors carefully consider these points when suggesting orchiectomy. They look at each patient’s health and what they prefer.
Benefits of Surgical Castration in Cancer Treatment
Surgical castration has many advantages of orchiectomy for prostate cancer patients. It is a proven way to manage hormone levels well.
Immediate Hormone Level Reduction
One big benefit is the rapid testosterone reduction it brings. This quick drop in testosterone can really slow down cancer growth.
Long-term Treatment Advantages
Surgical castration acts as a permanent hormone therapy. It means no need for ongoing meds. Patients enjoy a steady hormonal balance without daily treatments.
Cost Considerations Versus Other Treatments
Orchiectomy is often cheaper than other hormone therapies in the long run. The one-time procedure saves money on ongoing medication costs.
The Surgical Procedure: What to Expect
The surgical castration process starts with anesthesia. You can choose general anesthesia for full sleep or local anesthesia for numbness in the area.
During the testicular removal surgery, a small cut is made in the scrotum. The surgeon then removes the testicles. This usually takes about an hour and is done without staying overnight.
After surgery, you’ll get help with pain, infection, and any issues. You’ll need to rest and avoid hard activities for a few weeks.
| Anesthesia Type | Benefits | Potential Side Effects |
|---|---|---|
| General Anesthesia | Complete unconsciousness, no pain during surgery | Nausea, dizziness, longer recovery time |
| Local Anesthesia | Awake during procedure, quicker recovery | Limited pain control, possible discomfort |
Comparing Surgical Versus Chemical Castration
Understanding the differences between surgical and chemical castration is key when treating prostate cancer. Both methods aim to lower testosterone levels, which help cancer grow. But they do it in different ways.
Effectiveness Rates
Surgical castration is a permanent fix that lowers testosterone right away. It keeps hormone levels low without needing more treatment. Chemical castration, on the other hand, uses LHRH agonists to block testosterone production. It needs ongoing treatment to keep working.
Side Effect Profiles
The side effects of surgical and chemical castration are different. Surgical castration can cause immediate changes like lower libido and possible surgery problems. Chemical castration with LHRH agonists might lead to hot flashes, fatigue, and mood swings. It’s important to think about these side effects based on your health and what you prefer.
Cost Analysis
Cost is a big factor in choosing between surgical and chemical castration. Surgical castration costs less over time because it’s a one-time procedure. Chemical treatments, however, need ongoing medication, which can add up in cost. Patients and doctors need to consider these costs when deciding on treatment.
Physical and Emotional Recovery Process
Recovering from an orchiectomy takes time, both physically and emotionally. Right after, the focus is on controlling pain and taking care of the wound. This is to help the body heal properly.
As time goes on, hormone changes start to show. You might feel tired, lose muscle, and see changes in your body shape. It’s important to understand these changes to stay well in the long run.
The emotional side of surgical castration is also big. People often struggle with how they see their body and their masculinity. Mood swings and sadness are common as the body gets used to less testosterone.
Having a support system is key during recovery. Talking to mental health experts and joining groups can offer comfort and ways to deal with these feelings.
| Recovery Aspect | Strategies |
|---|---|
| Physical Recovery |
|
| Emotional Well-being |
|
| Hormone Adaptation |
|
Impact on Daily Life and Relationships
Having an orchiectomy changes your daily life and relationships. Knowing about these changes can make the transition smoother. It can also improve your overall well-being.
Physical Changes
Life after an orchiectomy brings physical changes. You might gain fat and lose muscle strength. Your sex life could change, making it harder to feel sexual and have erections.
Your energy levels might also change. You might need to adjust your daily activities to keep up with these changes.
Emotional Adjustments
Starting hormone therapy can be emotionally tough. You might feel mood swings, depression, and anxiety. These feelings come from your body adjusting to the new hormones.
Building your resilience and getting professional help can help. It can help you stay positive during treatment.
Partner Support Strategies
When you go through a castration, talking openly with your partner is key. Here are some ways to support each other:
- Have regular, honest talks about your feelings and worries.
- Go to couples counseling to work on intimacy and emotional connection.
- Join support groups together to share and learn from others.
These steps can make your relationship stronger. They ensure both of you feel supported and understood.
Alternative Treatment Options to Consider
Looking into prostate cancer treatment alternatives is key for a tailored care plan. Non-surgical hormone therapy is a big option. It lowers testosterone to slow cancer growth. Drugs like LHRH agonists and anti-androgens are often used.
Radiation therapy for prostate cancer is another good choice. It uses high-energy rays to kill cancer cells. The type of radiation therapy depends on the patient’s needs.
- LHRH Agonists: These drugs lower testosterone levels, stopping cancer from growing.
- Anti-Androgens: They block androgen receptors, stopping testosterone from helping cancer grow.
- Radiation Therapy: Uses targeted radiation to kill cancer cells without surgery.
Each treatment has its benefits and downsides. Hormone therapies might cause low libido and bone loss. Radiation therapy could lead to fatigue and skin issues. It’s vital to talk to a healthcare provider to find the best option for you.
| Treatment Option | Advantages | Disadvantages |
|---|---|---|
| Non-Surgical Hormone Therapy | Minimally invasive, effective in lowering testosterone | Potential side effects like fatigue and bone loss |
| Radiation Therapy for Prostate Cancer | Targets cancer cells precisely, preserves prostate | May cause fatigue and skin issues |
| LHRH Agonists | Significantly reduces testosterone levels | Possible hot flashes and decreased bone density |
Support Resources and Counseling Services
Facing an orchiectomy can be tough, but many support resources are here to help. Getting the right support can greatly improve your emotional and physical health.
Professional Support Networks
Professional support networks offer help from oncology social workers and psychologists. They give you personalized advice to manage stress and adjust to changes. Prostate cancer support services make sure you get care that fits your needs.
Patient Support Groups
Joining patient support groups lets you connect with others who understand. Sharing stories and advice helps build a sense of community. Psychological counseling for cancer patients in these groups helps with emotional healing.
Family Counseling Options
Orchiectomy affects not just the patient but the whole family. Family counseling gives loved ones a chance to share feelings and get support. Family support for orchiectomy patients helps strengthen relationships and ensures everyone can cope with treatment effects.
| Support Resource | Description | Benefits |
|---|---|---|
| Professional Support Networks | Access to social workers and psychologists specialized in oncology. | Personalized guidance and stress management. |
| Patient Support Groups | Community groups for sharing experiences and advice. | Emotional support and increased resilience. |
| Family Counseling Options | Sessions designed for family members of patients. | Strengthened relationships and coping strategies. |
Long-term Health Monitoring Requirements
After an orchiectomy, it’s key to keep up with post-orchiectomy health management. Regular visits to the doctor are crucial. They help spot any signs of cancer coming back early.
- PSA Tests: These track cancer activity by checking prostate-specific antigen levels.
- Bone Density Scans: They check bone health because of hormone changes.
- Cardiovascular Assessments: These look at heart health, affected by hormone loss.
- Hormone Level Monitoring: Regular blood tests keep hormone levels in check.
It’s important to manage side effects for a better quality of life. Patients should stay in close touch with their doctors. This ensures they get the best care and helps with ongoing hormone level monitoring.
| Monitoring Activity | Frequency |
|---|---|
| PSA Tests | Every 3-6 months |
| Bone Density Scans | Annually |
| Cardiovascular Assessments | Every 6 months |
| Hormone Level Monitoring | Monthly |
Living Successfully After Orchiectomy Treatment
Adjusting to life without testicles requires several steps. Start by eating well and exercising regularly. This helps keep your health in check and balances hormone levels.
Keeping sexual intimacy alive is possible with honest talks and understanding. Talk to doctors to find ways to maintain your sexual health and intimacy.
Mental health is key during this time. Look for counseling or join support groups. Connecting with others who get what you’re going through can be very helpful.
Find new ways to feel good about yourself and your masculinity. Engage in activities that make you happy. Many long-term survivors show that life after orchiectomy can be full and satisfying.
With the right approach and support, you can lead a fulfilling life without testicles.
FAQ
What is an orchiectomy and how does it relate to prostate cancer treatment?
Orchiectomy is a surgery that removes one or both testicles. It’s used in prostate cancer treatment to lower testosterone levels. This helps slow down hormone-sensitive prostate cancer growth.
How does testosterone affect the growth of prostate cancer?
Testosterone helps prostate cancer grow and spread. It fuels cancer cells. Lowering testosterone levels can slow cancer growth.
What are the benefits of choosing surgical castration over chemical methods?
Orchiectomy has benefits over chemical treatments. It immediately lowers hormone levels and is a permanent solution. It’s also more cost-effective than ongoing medication.
What can patients expect during the orchiectomy procedure?
Patients undergo surgery under local or general anesthesia. The testicles are removed. Post-surgery, they need to manage pain and watch for complications.
How does surgical castration compare to chemical castration in terms of effectiveness and side effects?
Both methods reduce testosterone levels. Orchiectomy is permanent, while chemical treatments need ongoing medication. Side effects are similar, but orchiectomy might have fewer long-term risks.
What support resources are available for patients undergoing orchiectomy?
Patients can find support through professional networks, support groups, and family counseling. These offer counseling, peer support, and help coping with emotional changes.
What are the long-term health monitoring requirements after an orchiectomy?
Patients need regular health checks. This includes PSA tests, bone density scans, and heart health assessments. Hormone levels must also be monitored to manage side effects.
How does orchiectomy impact daily life and relationships?
Orchiectomy causes physical and emotional changes. It affects body composition and sexual function. It also changes mood and self-perception. Open communication with partners is key to coping with these changes.
What alternative treatment options are available for prostate cancer besides orchiectomy?
Other options include hormone therapies, radiation, and prostatectomy. Each has its own benefits and drawbacks. Treatment plans should be tailored to individual needs.
How can patients maintain a good quality of life after undergoing orchiectomy?
Patients should focus on health with a balanced diet and exercise. Mental health is also crucial. Maintaining intimacy and seeking support are important. Joining survivorship programs and sharing experiences can also help.