Head and neck cancers are a diverse group of malignancies that can affect the mouth, throat, voice box, nasal cavity, and other nearby structures. Among the available treatments, radiation therapy for head and neck cancer plays a crucial role in both early-stage and advanced disease. It is often used as a primary treatment, in combination with surgery or chemotherapy, or as a method of relieving symptoms in advanced cases.
Over the years, advances in radiation delivery techniques have made this treatment more precise, effective, and tolerable. For patients and families navigating a cancer diagnosis, understanding how radiation therapy works, its potential side effects, and its role in survival outcomes can provide clarity and confidence in decision-making.
Definition and Overview
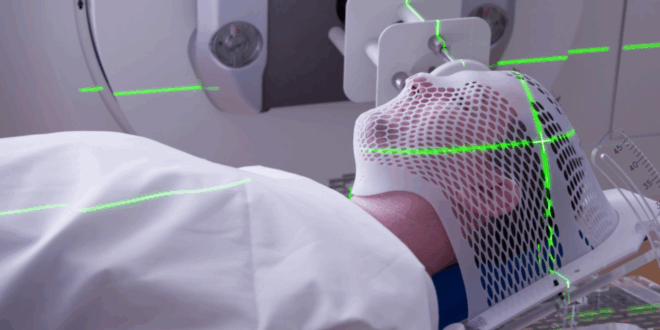
Radiation therapy for head and neck cancer uses high-energy beams, such as X-rays or protons, to destroy cancer cells. It can be applied externally using machines like linear accelerators (external beam radiation therapy) or internally with radioactive materials placed near the tumor (brachytherapy).
The treatment works by damaging the DNA of cancer cells, preventing them from growing and dividing. Because of advanced imaging and planning techniques, radiation can now be delivered with higher accuracy, minimizing harm to surrounding healthy tissues such as the salivary glands, jawbone, and throat.
Types
There are several types of radiation therapy for head and neck cancer, each suited to specific cases:
- External Beam Radiation Therapy (EBRT): The most common form, including 3D conformal radiation therapy (3D-CRT) and intensity-modulated radiation therapy (IMRT).
- Proton Therapy: Uses protons instead of X-rays for greater precision and less damage to nearby tissues.
- Stereotactic Body Radiotherapy (SBRT): Delivers high doses of radiation in fewer sessions, often for recurrent cancers.
- Brachytherapy: Radioactive sources are placed directly inside or near the tumor.
- Combination Therapy: Radiation used with chemotherapy (chemoradiation) for improved outcomes in advanced cases.
Causes and Risk Factors
Head and neck cancers develop due to multiple factors, many of which can influence treatment needs:
- Tobacco Use: Cigarettes, cigars, and chewing tobacco are leading causes.
- Alcohol Consumption: Heavy drinking combined with smoking increases risk significantly.
- Human Papillomavirus (HPV) Infection: Strongly linked to oropharyngeal cancers.
- Poor Oral Hygiene: Chronic irritation may contribute to cancer development.
- Occupational Exposure: Contact with certain chemicals, wood dust, or asbestos.
- Dietary Habits: Low fruit and vegetable intake is a potential factor.
- Genetics and Family History: May predispose individuals to certain cancers.
Symptoms and Early Warning Signs
Early detection plays an important role in treatment success. Symptoms to watch for include:
- Persistent sore throat or hoarseness
- Difficulty swallowing or breathing
- Unexplained lumps in the neck
- Chronic ear pain or hearing problems
- Mouth sores that do not heal
- Nosebleeds or persistent nasal congestion
- Unexplained weight loss and fatigue
These signs should prompt immediate medical evaluation, as timely radiation therapy for head and neck cancer can improve outcomes.
Diagnosis
Accurate diagnosis and staging are essential before beginning radiation treatment. Common diagnostic methods include:
- Physical Examination: Checking the oral cavity, throat, and neck lymph nodes.
- Endoscopy: Visual inspection with a flexible tube camera.
- Imaging Tests: CT, MRI, or PET scans to determine tumor size and spread.
- Biopsy: Tissue sampling to confirm cancer type.
- Molecular Testing: Identifying biomarkers such as HPV or p16 status to guide treatment.
These tests help oncologists design a personalized radiation therapy plan.
Treatment Options
Radiation therapy for head and neck cancer may be used alone or in combination with other treatments:
- Definitive Radiation Therapy: Primary treatment for patients who cannot undergo surgery.
- Post-Surgical Radiation Therapy: Reduces the risk of recurrence after tumor removal.
- Chemoradiation: Radiation combined with chemotherapy for advanced-stage disease.
- Palliative Radiation: Relieves pain, bleeding, or breathing difficulties in late-stage cancer.
Treatment duration typically ranges from five to seven weeks, with daily sessions.
Prevention and Lifestyle Recommendations
While not all cases are preventable, lifestyle changes can significantly reduce risk:
- Avoid smoking and limit alcohol consumption.
- Practice safe sex and consider HPV vaccination.
- Maintain good oral hygiene and regular dental check-ups.
- Eat a balanced diet rich in fruits and vegetables.
- Use protective equipment in workplaces with chemical exposure.
- Seek regular medical check-ups if at high risk.
These steps support both prevention and better recovery outcomes after treatment.
Prognosis and Survival Rates
The prognosis of head and neck cancer depends on cancer type, stage, HPV status, and overall health. HPV-positive cancers often respond better to radiation therapy and have higher survival rates compared to HPV-negative cancers.
On average, the five-year survival rate for localized head and neck cancers ranges from 60% to 80%, while advanced cases may have lower rates. The precision of modern radiation therapy for head and neck cancer has improved survival outcomes by reducing recurrence and sparing healthy tissues.
Latest Research and Innovations
Ongoing research is improving the effectiveness of radiation therapy for head and neck cancer:
- Adaptive Radiation Therapy: Adjusts radiation plans during treatment as tumors shrink.
- Proton Beam Advances: Provide greater accuracy and fewer side effects.
- Radiomics and AI Integration: Use imaging data to personalize radiation planning.
- Combined Immunotherapy and Radiation: Enhances the body’s immune response.
- Organ Preservation Strategies: Aim to treat cancer while maintaining speech and swallowing function.
These innovations are making treatment more targeted and less invasive.
Coping and Support for Patients
Radiation therapy can be challenging, both physically and emotionally. Patients benefit from comprehensive support systems:
- Nutritional Counseling: Helps manage side effects like difficulty swallowing or weight loss.
- Speech and Swallowing Therapy: Restores essential functions post-treatment.
- Psychological Support: Counseling and support groups reduce stress and depression.
- Palliative Care: Focuses on comfort, especially for advanced cases.
- Family and Caregiver Involvement: Provides emotional strength and practical assistance.
A holistic approach ensures that treatment addresses both medical and quality-of-life needs.
Conclusion
Radiation therapy for head and neck cancer remains a cornerstone of treatment, offering effective tumor control, improved survival, and symptom relief. With modern techniques, the balance between effectiveness and minimizing side effects has greatly improved, giving patients better chances for recovery and maintaining quality of life.
For patients and caregivers, understanding the role of radiation therapy, exploring innovative treatment options, and embracing supportive care can make the journey more manageable. As research continues to advance, radiation therapy will remain an essential tool in the fight against head and neck cancer.