Welcome to our comprehensive guide on transurethral resection of bladder tumor (TURBT), a highly effective procedure for treating bladder cancer. Bladder cancer is a type of malignancy that affects the bladder, a vital organ responsible for storing urine. TURBT, also known as transurethral bladder tumor resection, is a minimally invasive surgical technique used to remove bladder tumors.
Bladder tumors are abnormal growths that develop in the tissue lining the inside of the bladder. If left untreated, these tumors can lead to serious health complications. TURBT offers a promising solution for bladder cancer patients, providing a highly targeted approach to removing tumors while preserving bladder function.
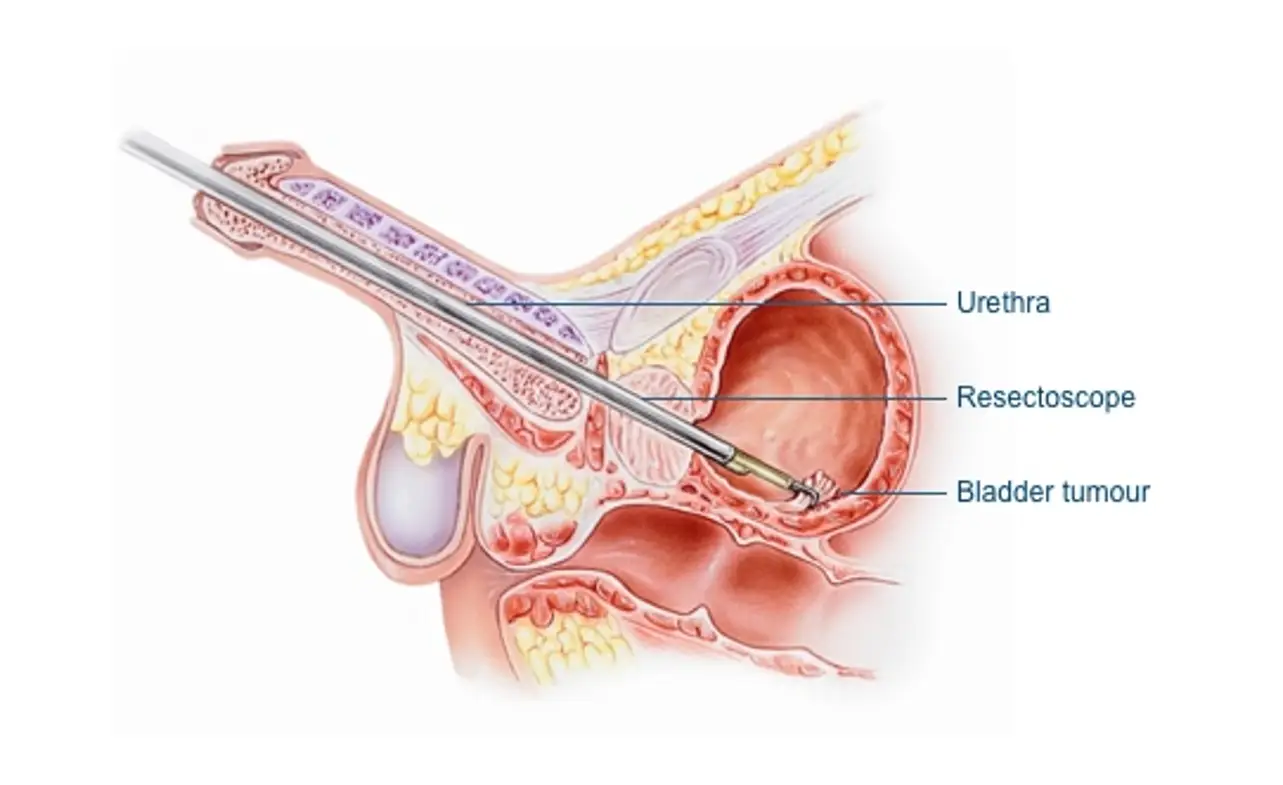
During a TURBT procedure, a urologist uses a special instrument called a resectoscope to remove the tumor from the bladder. This procedure offers several advantages, including the ability to examine the tumor and surrounding tissue under a microscope for accurate diagnosis, as well as the ability to remove tumors without making large incisions.
In this article, we will explore various aspects of transurethral resection of bladder tumors, including its benefits, the diagnosis of bladder cancer, the preparation for the TURBT procedure, the procedure itself, anesthesia options, and potential risks and complications. We will also discuss the recovery process, follow-up care, adjuvant treatment options, and the long-term outlook for patients who undergo TURBT.
Bladder cancer is a serious condition that requires timely and comprehensive treatment. If you or someone you know has been diagnosed with bladder cancer, understanding the options available, such as transurethral resection of a bladder tumor, can help make informed decisions and improve the chances of successful treatment. Let’s delve deeper into this innovative procedure and its role in combating bladder cancer.
Understanding Bladder Cancer
Bladder cancer is a malignant condition that originates in the cells of the bladder. It is one of the most common types of cancer, with thousands of new cases diagnosed each year.
Causes:
The exact cause of bladder cancer is not fully understood, but several risk factors have been identified. These include smoking, exposure to certain chemicals and toxins, chronic bladder inflammation, and genetic factors.
Symptoms:
Bladder cancer presents with various symptoms, including blood in the urine (hematuria), frequent urination, pain during urination, and lower back pain. However, it is important to note that these symptoms can also be caused by other conditions, so proper diagnosis is essential.
Prevalence:
Bladder cancer affects both men and women, but it is more common in men. According to the American Cancer Society, bladder cancer is the fourth most common cancer in men and the ninth most common in women in the United States.
Common Symptoms of Bladder Cancer
| Symptoms | Description |
|---|---|
| Blood in the urine (hematuria) | One of the most common signs of bladder cancer. It may be visible to the naked eye or detected during urinalysis. |
| Frequent urination | Feeling the need to urinate more often than usual, even with small amounts of urine. |
| Pain during urination | Experiencing discomfort or a burning sensation while passing urine. |
| Lower back pain | Unexplained pain in the lower back, often experienced on one side. |
To effectively treat bladder cancer, early detection and intervention are crucial. Transurethral resection of bladder tumor (TURBT) is a commonly used surgical procedure that plays a vital role in the management of bladder cancer. In the following sections, we will delve into the diagnosis, treatment, and recovery process associated with bladder cancer and TURBT.
Diagnosis of Bladder Cancer
Early diagnosis of bladder cancer is crucial for effective treatment and improved prognosis. Doctors employ a combination of diagnostic methods to accurately detect bladder cancer. These methods include:
- Cystoscopy: A procedure in which a thin, flexible tube with a camera is inserted into the bladder through the urethra. This allows the doctor to visually examine the bladder for any abnormalities or tumors.
- Imaging Tests: Imaging tests such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) may be used to assess the extent and spread of the cancer.
- Urine Tests: Urine tests, such as urine cytology and urine-based biomarker tests, can help identify abnormal cells or specific molecular markers that indicate the presence of bladder cancer.
The combination of these diagnostic methods allows healthcare professionals to accurately diagnose bladder cancer and determine the best course of treatment. Early detection increases the chances of successful treatment outcomes and improves overall prognosis.
| Diagnostic Method | Description |
|---|---|
| Cystoscopy | A procedure involving the insertion of a thin tube with a camera into the bladder to visualize any abnormalities or tumors. |
| Imaging Tests | Non-invasive imaging techniques such as ultrasound, CT scans, and MRI aid in assessing the extent and spread of bladder cancer. |
| Urine Tests | Laboratory tests, including urine cytology and biomarker analysis, to identify abnormal cells or molecular markers associated with bladder cancer. |
Introduction to Transurethral Resection of Bladder Tumor
Transurethral resection of bladder tumor (TURBT) is a common surgical procedure used for the treatment of bladder tumors, particularly those that are non-invasive or only slightly invasive. This minimally invasive procedure involves the removal of bladder tumors using a resectoscope, a specialized instrument inserted through the urethra.
TURBT is considered the gold standard for diagnosing and treating bladder tumors, as it allows for both diagnosis and treatment in a single procedure. It is performed under general or spinal anesthesia and typically does not require any external incisions, resulting in shorter hospital stays and faster recovery times for patients.
The TURBT Procedure
The TURBT procedure involves several key steps:
- Patient preparation: Before the procedure, the patient may need to undergo various tests, including blood work and imaging scans, to assess their overall health and the extent of the bladder tumor.
- Anesthesia administration: The patient is given anesthesia to ensure their comfort during the procedure. The type of anesthesia used may vary depending on the patient’s health, preferences, and the surgeon’s recommendations.
- Tumor identification: The surgeon inserts a cystoscope into the bladder through the urethra to visualize the tumor. A cystoscope is a thin tube with a light and a camera on the end, allowing the surgeon to see the tumor on a monitor.
- Tumor resection: Using a resectoscope with a wire loop or electrocautery device, the surgeon carefully removes the tumor or tumors from the bladder wall. The resectoscope can also be used to cauterize any bleeding vessels.
- Tissue sampling: Once the tumor is removed, the surgeon may collect tissue samples for further analysis to determine the tumor’s stage and grade.
- Bladder irrigation: After the tumor removal, the bladder is irrigated with a solution to remove any remaining tumor fragments and blood.
- Post-operative care: The patient is closely monitored in the recovery room and may be discharged on the same day or the following day, depending on their condition. They will receive instructions on post-operative care, including medication management and when to follow up with their healthcare provider.
By removing the tumor and obtaining tissue samples for analysis, TURBT helps in the accurate diagnosis, staging, and grading of bladder tumors. It also allows for the removal of small tumors and superficial layers of larger tumors, reducing the risk of tumor recurrence.
| TURBT Advantages | TURBT Considerations |
|---|---|
|
|
Patients need to discuss their specific case with their healthcare provider to determine if TURBT is the most appropriate treatment option for their bladder tumor.
Preparing for Transurethral Resection of Bladder Tumor
Before undergoing transurethral resection of bladder tumor (TURBT), patients need to follow specific preparations. This ensures a smooth and successful surgical experience. The preparations typically involve medical evaluations, lifestyle changes, and medication instructions.
Medical Evaluations
Patients scheduled for TURBT will undergo various medical evaluations to assess their overall health and suitability for the procedure. These evaluations may include:
- Physical examination: A thorough examination by a healthcare professional to evaluate the patient’s general health and identify any pre-existing conditions.
- Laboratory tests: Blood and urine tests may be conducted to assess kidney function, blood counts, and overall health status before surgery.
- Imaging tests: Depending on the individual case, additional imaging tests such as ultrasound, CT scans, or MRI scans may be ordered to evaluate the bladder tumor and surrounding structures.
Lifestyle Changes
Preparing for TURBT also involves making certain lifestyle changes to optimize the surgical outcome. These changes may include:
- Smoking cessation: Patients who smoke are advised to quit smoking to reduce the risk of complications during and after surgery.
- Dietary modifications: Following a healthy and balanced diet rich in fruits, vegetables, and lean proteins can help boost the immune system and promote healing.
- Exercise routine: Engaging in regular physical activity, as approved by the healthcare provider, can improve overall fitness and aid in a faster recovery post-surgery.
Medication Instructions
Patients will receive specific instructions regarding medication management in the period leading up to TURBT. These instructions may include:
- Discontinuation of certain medications: Patients may be advised to temporarily discontinue the use of blood-thinning medications or herbal supplements that can increase the risk of bleeding during surgery.
- Adjustment of current medications: Patients may need to adjust the dosage or timing of certain medications to ensure their safety and optimize surgical outcomes. It is important to follow the healthcare provider’s advice in this regard.
- New medication prescriptions: Based on individual needs, the healthcare provider may prescribe medications to prepare the bladder for surgery or to prevent urinary tract infections.
By carefully following the necessary preparations, patients can help improve the effectiveness and safety of transurethral resection of bladder tumors. These preparations help create a favorable environment for successful bladder tumor surgery, maximizing the chances of a positive outcome.
The TURBT Procedure
Transurethral resection of bladder tumor (TURBT) is a surgical procedure used to remove bladder tumors. It is a minimally invasive approach that offers several benefits, including faster recovery times and reduced risk of complications.
Step-by-step process of the TURBT procedure:
- Patient Preparation: The patient is positioned on a surgical table, and anesthesia is administered to ensure comfort throughout the procedure.
- Cystoscopy: A cystoscope, a thin tube with a light and camera at the end, is inserted through the urethra into the bladder. This allows the surgeon to visualize the tumor and surrounding tissue.
- Tumor Resection: A resectoscope, a specialized instrument with a wire loop, is then used to remove the tumor. The loop is carefully passed through the cystoscope and cuts the tumor away from the bladder wall.
- Tissue Sampling: Once the tumor is removed, small tissue samples may be taken for biopsy to determine the type and stage of cancer.
- Cauterization: After the tumor is removed, any bleeding vessels are cauterized, or sealed, to prevent excessive bleeding.
- Irrigation: The bladder is then irrigated with a saline solution to flush out any remaining tissue or blood.
- Stent Placement (if necessary): In some cases, a stent may be placed temporarily to ensure proper urine flow and prevent blockages during the healing process.
- Removal of Instruments: The cystoscope and resectoscope are carefully removed from the urethra, and the procedure is complete.
Overall, the TURBT procedure allows for targeted removal of bladder tumors while preserving bladder function. It is an effective treatment option for many bladder cancer patients.
| Advantages of TURBT | Disadvantages of TURBT |
|---|---|
| – Minimally invasive procedure | – Potential for tumor recurrence |
| – Shorter recovery time compared to open surgery | – Risk of bleeding and infection |
| – Preserves bladder function | – Possibility of bladder perforation |
| – Provides tissue samples for biopsy | – Temporary need for urinary catheter or stent |
Anesthesia Options for TURBT
During transurethral resection of bladder tumors (TURBT), different types of anesthesia can be used to ensure patient comfort and safety throughout the procedure. The choice of anesthesia depends on various factors, including the patient’s medical condition, the complexity of the surgery, and the surgeon’s recommendation.
1. Local Anesthesia:
Local anesthesia involves the injection of medication to numb a specific area or region of the body. In the case of TURBT, local anesthesia can be administered to the urinary tract, providing pain relief during the procedure. This type of anesthesia allows the patient to remain awake and aware during the surgery, without feeling pain.
2. Spinal Anesthesia:
Spinal anesthesia is an option for TURBT that involves the injection of anesthesia medication into the fluid surrounding the spinal cord. This results in temporary numbness in the lower body, allowing the patient to remain conscious but free from pain. Spinal anesthesia is particularly useful for longer surgeries or when multiple procedures are performed at the same time.
3. General Anesthesia:
General anesthesia is often used for more complex or prolonged TURBT surgeries. It involves the administration of medication that induces a state of unconsciousness, ensuring that the patient feels no pain or discomfort during the procedure. General anesthesia requires careful monitoring of vital signs by an anesthesiologist to ensure the patient’s safety and optimal surgical conditions.
Each type of anesthesia has its advantages and considerations. Local anesthesia is minimally invasive, avoids potential side effects associated with general anesthesia, and allows for a faster recovery. Spinal anesthesia provides effective pain relief and can be combined with sedation for increased patient comfort. General anesthesia ensures complete unconsciousness and pain control during surgery.
The choice of anesthesia for TURBT is made by the healthcare team based on the patient’s medical history, surgical requirements, and the expertise of the anesthesia provider. Before undergoing TURBT, patients will discuss with their healthcare team to determine the most suitable anesthesia option for their specific situation.
Potential Risks and Complications of TURBT
Transurethral resection of bladder tumor (TURBT) is a commonly performed procedure for the treatment of bladder cancer. While it offers numerous benefits, it is important to be aware of the potential risks and complications associated with this surgery.
Bleeding:
- TURBT can cause bleeding, both during and after the procedure. In some cases, patients may experience blood in their urine for a few days following surgery.
- Significant bleeding may require further medical intervention, such as bladder irrigation or blood transfusion.
Infection:
- There is a risk of infection following TURBT, especially if proper precautions are not taken.
- Patients may be prescribed antibiotics to prevent infection.
- It is important to report any signs of infection, such as increased pain, fever, or urinary tract symptoms.
Bladder Perforation:
- In rare cases, TURBT can result in bladder perforation, which is a hole in the bladder wall.
- This complication may require surgical repair.
- Bladder perforation can cause urine leakage, infection, and other complications.
Urinary Retention:
- Following TURBT, some patients may experience difficulty in emptying their bladder.
- Temporary urinary retention can occur due to swelling or spasms of the bladder.
- In some cases, a urinary catheter may be temporarily inserted to aid in emptying the bladder.
Other Potential Complications:
- Scar tissue formation in the bladder may cause bladder contracture, leading to urinary flow problems.
- There is a risk of damage to surrounding structures, such as the urethra or ureter.
- Rarely, TURBT can result in complications like blood clots, urinary incontinence, or erectile dysfunction.
Patients need to discuss these potential risks and complications with their healthcare provider before undergoing TURBT. While the benefits of TURBT in treating bladder cancer are significant, a thorough understanding of the procedure and its potential risks is crucial for informed decision-making.
Recovery Process After TURBT
After undergoing transurethral resection of bladder tumor (TURBT), the recovery phase plays a crucial role in ensuring a successful outcome. This section provides guidance on the postoperative care and recovery process for patients who have undergone this procedure. It covers important aspects such as pain management, catheter use, and resuming normal activities.
1. Pain Management
Pain management is a key consideration during the recovery period. Following TURBT, it is common to experience some discomfort or pain in the lower abdomen or urinary tract. Your healthcare team will provide appropriate pain relief medication to ensure your comfort and manage any postoperative pain.
2. Urinary Catheter
During the recovery process, you may have a urinary catheter in place. This catheter allows your body to heal by diverting urine away from the surgical site. Your healthcare team will guide the proper care and management of the catheter, including instructions for cleaning and preventing infection. It is important to follow these guidelines carefully for optimal recovery.
3. Monitoring and Follow-Up
Your healthcare team will schedule regular follow-up appointments to monitor your progress and ensure that you are healing well. These appointments may include physical examinations, urine tests, and imaging tests to assess the bladder and monitor for any signs of recurrence. It is crucial to attend these appointments and communicate any concerns or symptoms you may experience.
4. Resuming Normal Activities
As you progress through the recovery phase, your healthcare team will guide you when it is appropriate to resume normal activities. This may include recommendations for gradually increasing physical activity, returning to work, and resuming hobbies or exercise. It is important to follow these instructions to promote healing and avoid complications.
5. Support and Rehabilitation
During the recovery process, it is normal to experience physical and emotional challenges. The support of your healthcare team, as well as friends and family, can greatly contribute to your overall well-being. Additionally, if needed, your healthcare team may recommend resources or rehabilitation programs to assist with recovery, including physical therapy or counseling services.
| Recovery Process After TURBT | Key Points |
|---|---|
| Pain Management | – Ensure proper pain relief medication – Communicate any discomfort or pain to your healthcare team |
| Urinary Catheter | – Follow the care instructions provided by your healthcare team – Prevent infection through proper catheter hygiene |
| Monitoring and Follow-Up | – Attend regular follow-up appointments to assess healing and detect any signs of recurrence – Communicate any concerns or symptoms |
| Resuming Normal Activities | – Gradually increase physical activity as advised – Follow guidelines for returning to work and hobbies |
| Support and Rehabilitation | – Seek support from the healthcare team, friends, and family – Access resources or rehabilitation programs if needed |
Follow-Up Care and Monitoring
After undergoing transurethral resection of a bladder tumor (TURBT), regular follow-up care and monitoring are crucial for the long-term management of bladder cancer. This includes close surveillance to detect any potential recurrences or the development of new tumors.
Patients who have undergone TURBT should schedule regular check-ups with their healthcare provider to monitor their progress and ensure any changes in their condition are promptly addressed. These follow-up appointments typically include:
- Physical examination to assess overall health and any signs of tumor recurrence
- Cystoscopy, is a procedure that allows the doctor to visually inspect the inside of the bladder using a thin tube-like instrument called a cystoscope
- Urine tests to check for any abnormalities or the presence of cancer cells
- Imaging tests such as CT scans or ultrasounds to evaluate the bladder and surrounding structures for any signs of cancer recurrence or metastasis
During the follow-up period, patients should also be vigilant about reporting any symptoms or changes they experience, such as blood in the urine, increased frequency of urination, or pain. Early detection of recurrent tumors is essential for ensuring timely intervention and optimal treatment outcomes.
Furthermore, healthcare providers may recommend additional adjuvant treatments, such as intravesical chemotherapy or immunotherapy, as a preventive measure to reduce the risk of tumor recurrence. These treatments are often administered directly into the bladder to target any residual cancer cells and enhance the chances of long-term remission.
In conclusion, TURBT follow-up and bladder tumor surveillance play a vital role in the ongoing management of bladder cancer. Regular check-ups and monitoring enable early detection of recurrences or new tumors, allowing for timely interventions and improved treatment outcomes.
Adjuvant Treatment Options
After undergoing transurethral resection of bladder tumor (TURBT), patients may require additional therapies to prevent tumor recurrence and improve long-term outcomes. Adjuvant treatment options, such as intravesical chemotherapy and immunotherapy, are commonly recommended as part of a comprehensive bladder cancer treatment plan.
Intravesical chemotherapy: This adjuvant treatment involves the placement of anti-cancer drugs directly into the bladder, where the tumor is removed. The chemotherapy drugs target any remaining cancer cells and help prevent their growth and spread. Commonly used drugs include mitomycin-C and Bacillus Calmette-Guérin (BCG), an immunotherapy drug that also stimulates the immune system.
Immunotherapy: Immunotherapy harnesses the power of the patient’s immune system to recognize and attack cancer cells. One commonly used immunotherapy drug for bladder cancer is BCG, which stimulates an immune response in the bladder. BCG is administered via intravesical installation, directly into the bladder, after TURBT. Other immunotherapy drugs, such as pembrolizumab and atezolizumab, may be used in certain cases.
Comparing Intravesical Chemotherapy and Immunotherapy for Adjuvant Treatment
| Treatment | Benefits | Considerations |
|---|---|---|
| Intravesical Chemotherapy |
|
|
| Immunotherapy (BCG) |
|
|
Patients need to discuss the potential benefits and considerations of these adjuvant treatments with their healthcare team. The choice of treatment will depend on various factors, including the stage and grade of the tumor, the overall health of the patient, and their individual preferences.
Potential Side Effects and Long-Term Implications
Transurethral resection of bladder tumor (TURBT) is an effective procedure for treating bladder cancer. However, like any surgical intervention, it may have potential side effects and long-term implications that patients should be aware of.
Urinary Incontinence
One potential side effect of TURBT is urinary incontinence, which is the involuntary leakage of urine. This can occur due to damage to the urinary sphincter muscles during the surgery. While this side effect is generally temporary, some patients may experience long-term or permanent urinary incontinence.
Erectile Dysfunction
In male patients, TURBT surgery may lead to erectile dysfunction, the inability to achieve or maintain an erection sufficient for sexual activity. This can happen if the nerves responsible for erection are damaged during the procedure. The likelihood of experiencing erectile dysfunction depends on various factors, including the extent of the surgery and the individual’s overall health.
Impact on Fertility
For patients who wish to have children in the future, TURBT surgery may have implications on fertility. In some cases, the removal of bladder tumors may require the removal of a portion of the bladder, which can affect the storage and passage of urine. This may impact fertility, particularly if the surgery involves the removal of reproductive organs or nearby structures.
Other Side Effects
In addition to urinary incontinence, erectile dysfunction, and impacts on fertility, other potential side effects of TURBT surgery may include:
- Bleeding
- Infection
- Bladder spasms
- Urinary tract infections
- Scarring
Patients need to discuss these potential side effects and long-term implications with their healthcare team. Each individual’s experience may vary, and healthcare professionals can provide personalized information and guidance based on the patient’s specific situation.
| Side Effect | Description |
|---|---|
| Urinary Incontinence | Involuntary leakage of urine |
| Erectile Dysfunction | Inability to achieve or maintain an erection |
| Impact on Fertility | Implications on reproductive capacity |
| Bleeding | Excessive or prolonged bleeding |
| Infection | Infection at the surgical site or in the urinary tract |
| Bladder spasms | Involuntary contractions of the bladder |
| Urinary tract infections | Infections affecting the urinary system |
| Scarring | Formation of scar tissue in the bladder |
TURBT Success Rates and Prognosis
Transurethral resection of bladder tumor (TURBT) is a widely used procedure for treating bladder cancer. The success rates and prognosis associated with TURBT can vary depending on several factors, including the stage and grade of the tumor.
Factors Influencing Success Rates
Stage of the Tumor: The stage of the tumor at the time of TURBT plays a crucial role in determining the success rates. Earlier-stage tumors have better outcomes compared to advanced-stage tumors.
Grade of the Tumor: The grade of the tumor, which is an indicator of its aggressiveness, also influences the success rates. Low-grade tumors generally have higher success rates than high-grade tumors.
Complete Removal of the Tumor: The ability to completely remove the tumor during TURBT is essential for achieving successful outcomes. If any cancerous cells are left behind, it can lead to recurrence or progression of the disease.
Prognosis After TURBT
The prognosis after TURBT depends on various factors, such as the stage and grade of the tumor, as well as the patient’s overall health and response to treatment.
Tumor Stage: The stage of the tumor is a critical prognostic factor. Early-stage tumors have better prognoses, with higher chances of successful treatment and long-term survival. Advanced-stage tumors may have a lower prognosis due to a higher risk of recurrence or metastasis.
Tumor Grade: The grade of the tumor also affects the prognosis. Low-grade tumors tend to have a more favorable prognosis compared to high-grade tumors.
Response to Treatment: How well a patient responds to TURBT and any subsequent treatments can impact the prognosis. Adequate response to treatment increases the likelihood of disease control and improves long-term outcomes.
Overall Health: The patient’s overall health, including any pre-existing medical conditions, can influence the prognosis. Good overall health and well-being may enhance the success of the treatment and contribute to better long-term outcomes.
| TUMBT Success Rates and Prognosis | Factors Influencing Success Rates |
|---|---|
| Stage of the Tumor | Earlier-stage tumors have better outcomes compared to advanced-stage tumors. |
| Grade of the Tumor | Low-grade tumors generally have higher success rates than high-grade tumors. |
| Complete Removal of the Tumor | The ability to completely remove the tumor during TURBT is essential for achieving successful outcomes. |
Alternative Treatment Options for Bladder Cancer
When it comes to bladder cancer, transurethral resection of bladder tumor (TURBT) is a common surgical option. However, there are alternative treatments available for bladder cancer patients, especially for those who are unable to undergo surgery or wish to explore non-surgical options. These alternative treatment options can be used as standalone therapies or in conjunction with TURBT, depending on the individual needs and preferences of the patient.
Radiation Therapy:
Radiation therapy is a non-surgical treatment for bladder cancer that uses high-energy beams to target and destroy cancer cells. It can be delivered externally using a machine called a linear accelerator or internally using radioactive materials placed directly in the bladder. Radiation therapy is often used after TURBT to eliminate any remaining cancer cells and reduce the risk of recurrence.
Chemotherapy:
Chemotherapy involves the use of drugs to kill cancer cells throughout the body. It can be administered orally or intravenously and may be used before or after TURBT. Chemotherapy drugs can be effective in treating advanced or metastatic bladder cancer, as well as preventing the spread of cancer cells.
Immunotherapy:
Immunotherapy is a type of treatment that helps the body’s immune system fight against cancer. It works by stimulating the immune system to recognize and attack cancer cells. Immunotherapy drugs, such as checkpoint inhibitors, are now being used in the treatment of bladder cancer and have shown promising results.
Targeted Therapy:
Targeted therapy is a treatment approach that specifically targets the abnormalities present in cancer cells. These therapies work by blocking the signals that cancer cells need to divide and grow. Targeted therapy can be used in combination with other treatments, including TURBT, to enhance the effectiveness of the overall treatment plan.
Bladder cancer patients need to consult with their healthcare provider to determine the most appropriate treatment options for their specific case. Each alternative treatment option has its benefits and considerations, and the choice may depend on factors such as the stage and grade of the cancer, the overall health of the patient, and individual treatment goals.
Support and Resources for Bladder Cancer Patients
Receiving a bladder cancer diagnosis can be a challenging and overwhelming experience. However, there are numerous support networks, organizations, and resources available to provide assistance and guidance to bladder cancer patients and their loved ones.
One vital aspect of coping with bladder cancer is accessing emotional support. Dealing with a cancer diagnosis can have a significant emotional impact, and having a network of understanding individuals can be invaluable. Support groups, both in-person and online, offer a platform for patients to connect with others who have similar experiences. These groups provide a safe space to share thoughts, fears, and victories, fostering a sense of community and understanding.
Bladder cancer patients also benefit from educational resources that offer in-depth information related to their condition. Organizations such as the American Cancer Society and the Bladder Cancer Advocacy Network provide comprehensive educational materials, including brochures, websites, and videos, which cover topics ranging from treatment options to coping strategies. These resources empower patients to make informed decisions about their care and improve their overall well-being.
Practical assistance is another essential component of bladder cancer support. Many organizations offer programs that connect patients with services and resources to help them navigate their cancer journey. Support may include assistance with transportation to medical appointments, financial aid for treatment-related expenses, and guidance in accessing appropriate healthcare professionals and facilities.
Here is a list of some reputable organizations that provide support and resources for bladder cancer patients:
- American Cancer Society – www.cancer.org
- Bladder Cancer Advocacy Network – www.bcan.org
- Bladder Cancer Canada – www.bladdercancercanada.org
- The Urology Care Foundation – www.urologyhealth.org
Resources for Bladder Cancer Support
| Organization | Website |
|---|---|
| American Cancer Society | www.cancer.org |
| Bladder Cancer Advocacy Network | www.bcan.org |
| Bladder Cancer Canada | www.bladdercancercanada.org |
| The Urology Care Foundation | www.urologyhealth.org |
By utilizing these support networks, organizations, and resources, bladder cancer patients can find the help they need to navigate their cancer journey effectively. Whether it’s emotional support, educational materials, or practical assistance, these resources empower patients to face the challenges of bladder cancer with resilience and hope.
Conclusion
In conclusion, transurethral resection of bladder tumors (TURBT) is a highly effective and minimally invasive procedure for the treatment of bladder cancer. Throughout this article, we have discussed the various aspects of TURBT, including its benefits, the procedure itself, and the recovery process.
TURBT offers numerous advantages, such as the ability to remove bladder tumors without the need for open surgery, reduced hospital stays, and faster recovery times. It plays a crucial role in the diagnosis, treatment, and management of bladder cancer, particularly in early-stage and non-muscle invasive cases.
By utilizing advanced instruments and techniques, TURBT allows for precise tumor removal while minimizing damage to healthy bladder tissue. It is complemented by comprehensive follow-up care and monitoring to detect any signs of recurrence or new tumors. In cases where adjuvant treatments are necessary, TURBT can be combined with other therapies to optimize outcomes and improve long-term prognosis.
Patients undergoing TURBT should work closely with their healthcare team to ensure proper preparation, adherence to post-operative care instructions, and regular follow-up appointments. By taking these steps, individuals can maximize the success of their treatment and enhance their overall quality of life.
FAQ
What is transurethral resection of bladder tumor (TURBT)?
Transurethral resection of bladder tumor (TURBT) is a surgical procedure used to remove cancerous tumors from the bladder. It is a minimally invasive technique that involves using a resectoscope to remove the tumor through the urethra.
How is TURBT performed?
TURBT is performed using a specialized instrument called a resectoscope. The resectoscope is inserted through the urethra and guided to the bladder. The tumor is then removed using a wire loop or laser, and the area is cauterized to control bleeding.
What are the benefits of TURBT?
TURBT offers several benefits for bladder cancer patients. It is a minimally invasive procedure that allows for the removal of cancerous tumors without the need for open surgery. It has a shorter recovery time compared to traditional surgery and can help preserve bladder function.
How do I prepare for TURBT?
To prepare for TURBT, you may need to undergo medical evaluations and tests to assess your overall health and bladder condition. Your healthcare provider will provide specific instructions on medication usage, dietary restrictions, and any lifestyle changes that may be necessary.
What are the potential risks and complications of TURBT?
Like any surgical procedure, TURBT carries some risks and potential complications. These can include bleeding, infection, bladder perforation, and scarring. Your healthcare provider will discuss these risks with you and take steps to minimize them during the procedure.
What is the recovery process like after TURBT?
The recovery process after TURBT can vary depending on individual factors, such as the extent of the procedure and overall health. You may experience some discomfort and urinary symptoms in the days following surgery. Your healthcare provider will guide pain management, bladder care, and when you can resume normal activities.
Will I need follow-up care after TURBT?
Yes, follow-up care is essential after TURBT. Regular monitoring and surveillance are important to detect any recurrence or new tumors. Your healthcare provider may recommend periodic cystoscopies, imaging tests, and urine tests to ensure early detection and appropriate management.
Are there alternative treatment options for bladder cancer?
Yes, there are alternative treatment options for bladder cancer. These can include radiation therapy, chemotherapy, immunotherapy, and targeted therapy. They may be used alone or in combination with TURBT, depending on factors such as the stage and grade of the cancer.
Where can I find support and resources for bladder cancer?
There are various support networks, organizations, and resources available to bladder cancer patients and their families. These can provide emotional support, educational materials, and practical assistance. Your healthcare provider can provide recommendations or referrals to relevant resources.