Nivolumab Pancreatic Cancer: Symptoms, Causes, Treatment, Prognosis
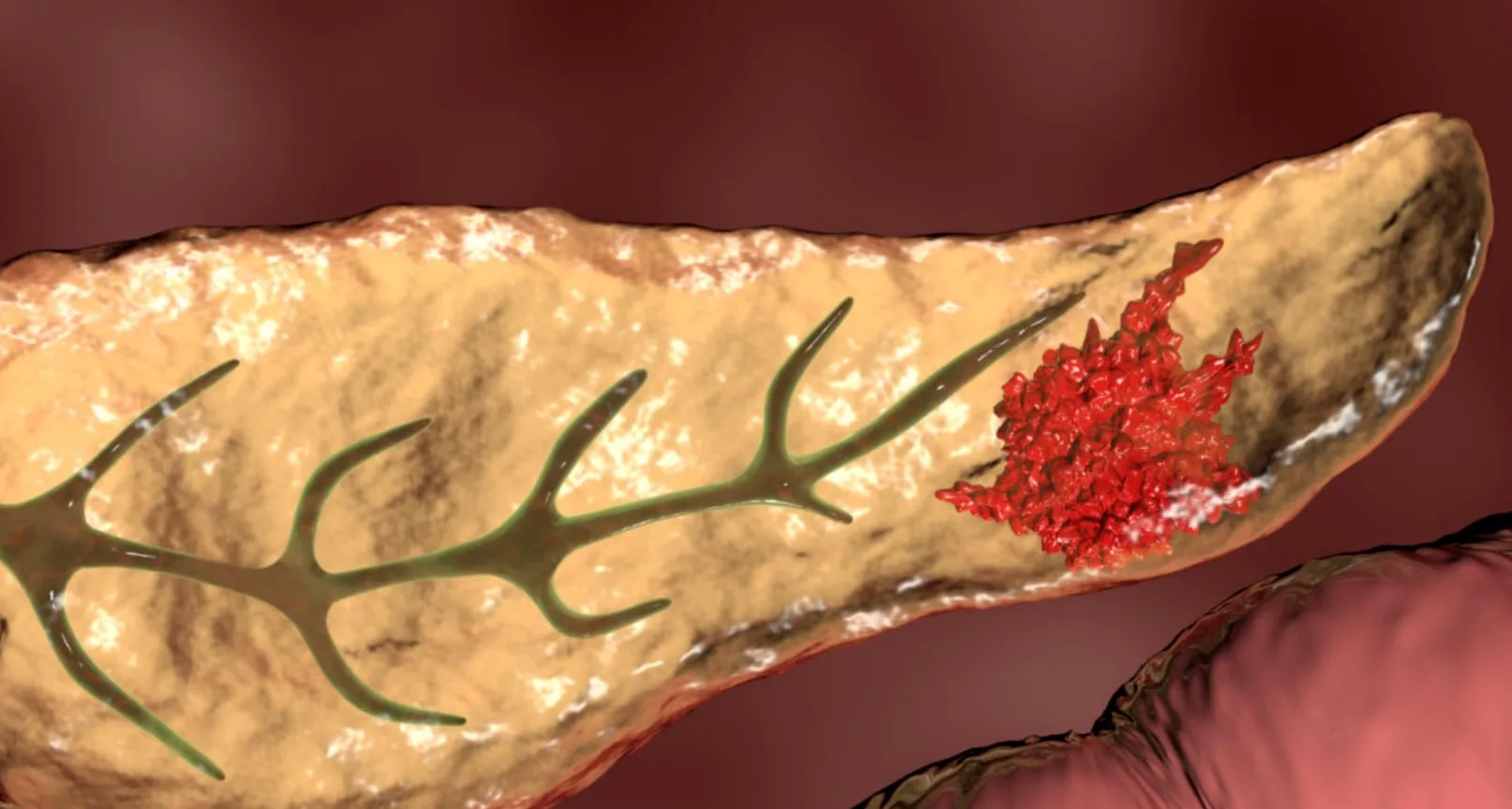
Pancreatic cancer is one of the most aggressive and difficult-to-treat cancers worldwide. Its late diagnosis and resistance to traditional treatments make it a leading cause of cancer-related deaths. In recent years, researchers have been exploring innovative therapies that go beyond chemotherapy and radiation, focusing instead on immunotherapy approaches.
One promising option is nivolumab, an immune checkpoint inhibitor that has shown potential in various cancers. When it comes to nivolumab pancreatic cancer, ongoing studies are evaluating its role in improving outcomes for patients. This article provides a detailed overview of nivolumab in pancreatic cancer treatment, including causes, diagnosis, survival rates, research, and supportive care strategies.
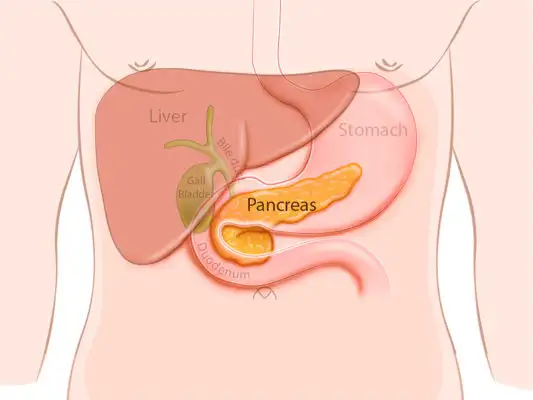
Definition and Overview
Nivolumab is a type of immunotherapy classified as a PD-1 inhibitor. It works by blocking the programmed death-1 (PD-1) pathway, allowing the immune system to better recognize and attack cancer cells. In the context of pancreatic cancer, nivolumab is not yet a standard treatment but is being tested in clinical trials to assess its effectiveness. Early evidence suggests that combining nivolumab with other therapies may enhance patient response rates.
Types
Pancreatic cancer can be divided into two main types:
- Exocrine tumors – The most common type, including pancreatic ductal adenocarcinoma, which accounts for over 90% of cases.
- Endocrine tumors (neuroendocrine tumors) – Less common but generally less aggressive, arising from hormone-producing cells.
Nivolumab research primarily focuses on pancreatic ductal adenocarcinoma due to its poor prognosis and limited treatment success with conventional therapies.
Causes and Risk Factors
The exact cause of pancreatic cancer is still unclear, but several risk factors have been identified:
- Genetic mutations and family history of pancreatic or other cancers
- Chronic pancreatitis
- Smoking and excessive alcohol consumption
- Obesity and poor dietary habits
- Age (most patients are over 60)
- Certain inherited syndromes such as Lynch syndrome or BRCA mutations
These risk factors may increase the likelihood of developing pancreatic cancer, making early screening essential for high-risk individuals.
Symptoms and Early Warning Signs
Pancreatic cancer often develops silently, with symptoms appearing only in advanced stages. Common warning signs include:
- Persistent abdominal pain or back pain
- Unexplained weight loss
- Jaundice (yellowing of the skin and eyes)
- Loss of appetite or nausea
- Dark urine and pale stools
- Fatigue and weakness
Because these symptoms overlap with many other conditions, pancreatic cancer is frequently diagnosed late.
Diagnosis
Diagnosing pancreatic cancer involves multiple approaches:
- Imaging tests such as CT scans, MRI, and endoscopic ultrasound
- Biopsy to confirm cancer cells
- Blood tests including CA 19-9, a tumor marker
- Genetic testing for mutations that may guide targeted therapies
Accurate diagnosis is critical to determine whether patients may be eligible for treatments such as nivolumab or other immunotherapy-based clinical trials.
Treatment Options
Traditional treatments for pancreatic cancer include surgery, chemotherapy, and radiation therapy. However, survival rates remain low, prompting the exploration of new methods.
- Chemotherapy: Standard drugs like gemcitabine and FOLFIRINOX are commonly used.
- Radiation therapy: Helps control tumor growth and reduce symptoms.
- Targeted therapy: Designed for patients with specific genetic mutations.
- Immunotherapy (Nivolumab): Still under research for pancreatic cancer, nivolumab may help the immune system fight tumor cells more effectively. Some studies suggest that combining nivolumab with chemotherapy or other checkpoint inhibitors may provide better outcomes.
Prevention and Lifestyle Recommendations
While not all cases of pancreatic cancer can be prevented, certain lifestyle choices may reduce risk:
- Avoid smoking and limit alcohol consumption
- Maintain a healthy weight through balanced diet and exercise
- Eat more fruits, vegetables, and whole grains
- Manage chronic conditions like diabetes and pancreatitis
- Undergo regular screenings if you have a strong family history or genetic risk
These preventive steps can support overall health and potentially lower pancreatic cancer risk.
Prognosis and Survival Rates
Pancreatic cancer has one of the lowest survival rates among cancers, with a five-year survival rate of around 10%. This is largely due to late-stage diagnoses and limited treatment responses. However, ongoing research into nivolumab pancreatic cancer offers new hope. Clinical trials suggest that select patients, especially those with certain genetic mutations or tumor characteristics, may respond more favorably to immunotherapy.
Latest Research and Innovations
Recent innovations in pancreatic cancer treatment focus heavily on immunotherapy and personalized medicine. Key developments include:
- Clinical trials combining nivolumab with chemotherapy or radiation
- Research into biomarkers that predict response to PD-1 inhibitors
- Combination therapies involving nivolumab and CTLA-4 inhibitors
- Exploration of personalized cancer vaccines in synergy with immunotherapy
These advancements highlight the growing role of nivolumab and related treatments in the fight against pancreatic cancer.
Coping and Support for Patients
Living with pancreatic cancer can be overwhelming for both patients and families. Emotional, psychological, and physical support is crucial. Patients are encouraged to:
- Join cancer support groups to connect with others
- Seek counseling for mental health and stress management
- Discuss palliative care options to improve quality of life
- Explore clinical trials for access to innovative treatments like nivolumab
- Rely on family, friends, and professional caregivers for daily assistance
Comprehensive support can make a significant difference in coping with the disease.
Conclusion
Pancreatic cancer remains one of the most challenging cancers to treat, but emerging therapies such as nivolumab provide new possibilities for improved outcomes. While it is not yet a standard treatment, ongoing research continues to explore its potential in combination therapies and specific patient groups.
For patients and caregivers, staying informed about nivolumab pancreatic cancer and other innovative treatments can empower decision-making and provide hope. With continued advancements, the future of pancreatic cancer care may bring better survival rates and improved quality of life.
FAQ
1. What is nivolumab used for in pancreatic cancer?
Nivolumab is being studied as an immunotherapy option to help the immune system recognize and fight pancreatic cancer cells.
2. Is nivolumab approved for pancreatic cancer treatment?
Currently, nivolumab is not FDA-approved specifically for pancreatic cancer but is under clinical investigation.
3. Who may benefit from nivolumab pancreatic cancer therapy?
Patients with certain genetic mutations or those enrolled in clinical trials may benefit more from nivolumab-based treatments.
4. Are there side effects of nivolumab?
Yes. Side effects may include fatigue, skin rash, diarrhea, and immune-related complications such as thyroid or liver inflammation.
5. How can patients access nivolumab for pancreatic cancer?
Patients can participate in clinical trials or consult with oncologists about compassionate use programs and ongoing research opportunities.