Pancreatic Cancer Stages of Dying: A Complete Guide for Patients
Pancreatic cancer is widely recognized as one of the most aggressive and challenging cancers to diagnose and treat. Many patients and families search online for information about pancreatic cancer stages of dying to better understand what to expect, how symptoms may progress, and how to prepare emotionally and physically during this difficult time. Having clear, compassionate, and accurate information can help reduce fear and uncertainty.
Understanding the stages of dying in pancreatic cancer is not about giving up hope, but about empowering patients and caregivers with knowledge. This guide explains the medical aspects, symptom progression, treatment approaches, and supportive care options, while also addressing emotional and practical needs. Our goal is to provide a professional, informative, and empathetic resource optimized for clarity and relevance.
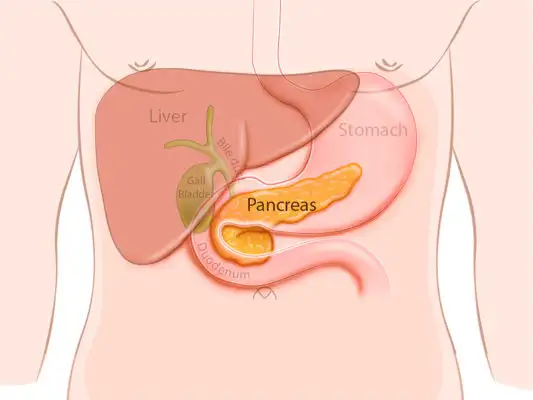
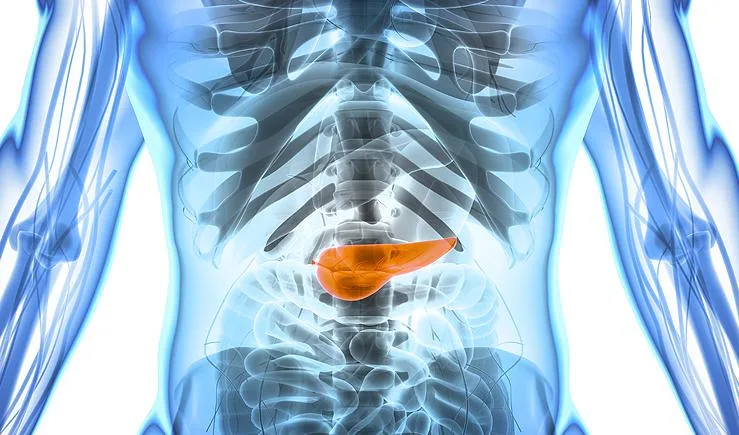
Definition and Overview
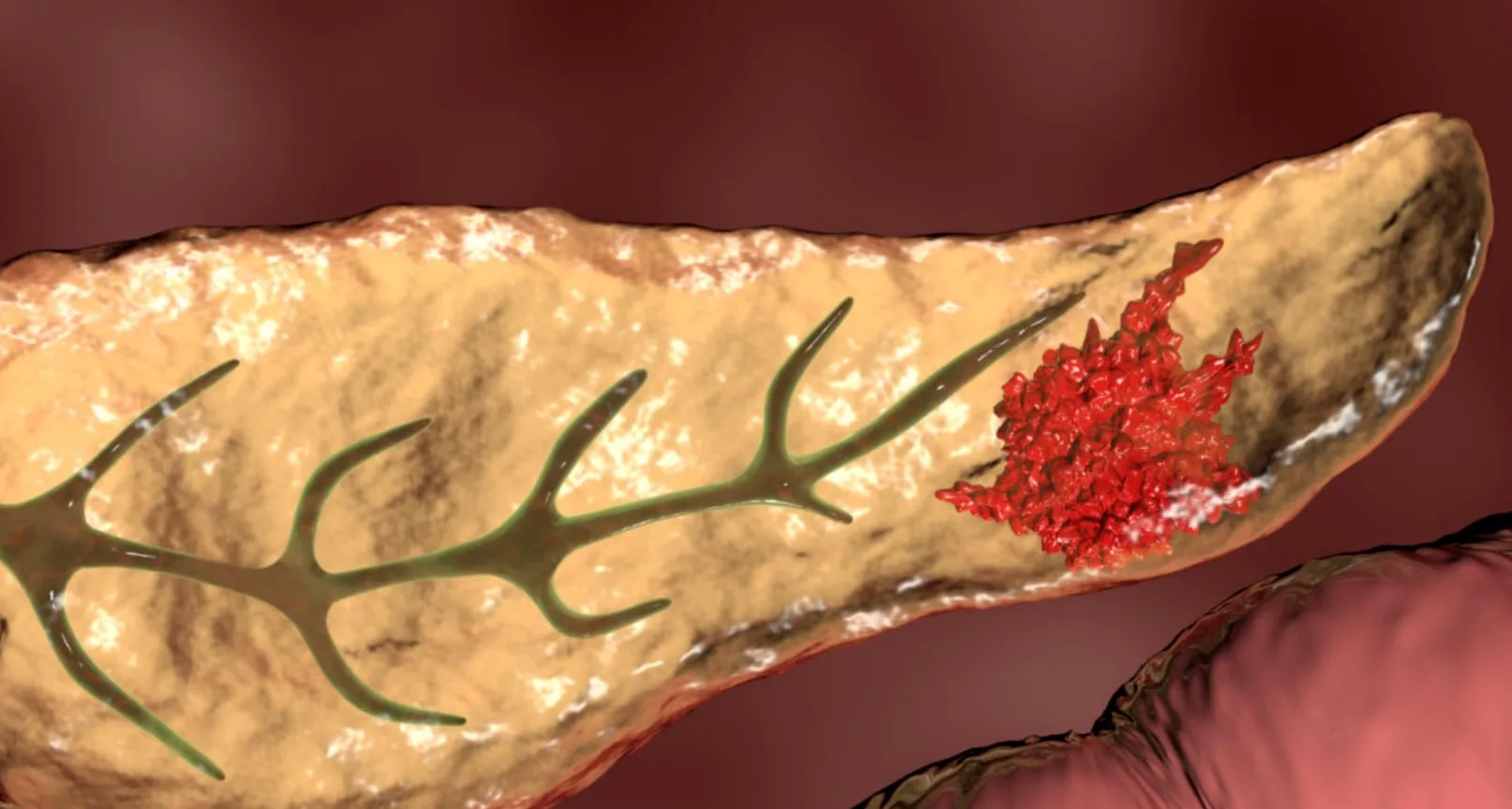
Pancreatic cancer develops when abnormal cells grow uncontrollably in the pancreas, an organ located behind the stomach that plays a key role in digestion and blood sugar regulation. The disease often goes undetected in its early stages due to vague or absent symptoms.
The term pancreatic cancer stages of dying refers to the advanced phase of the illness, typically stage IV or end-stage pancreatic cancer, when the disease has spread extensively and the focus of care shifts from curative treatment to comfort, symptom control, and quality of life.
Types
There are several types of pancreatic cancer, each with different behaviors and outcomes:
-
Pancreatic ductal adenocarcinoma (PDAC): The most common and aggressive type, accounting for over 90% of cases.
-
Neuroendocrine tumors (NETs): Less common and often slower-growing.
-
Acinar cell carcinoma: Rare and biologically distinct.
-
Mucinous and cystic tumors: Some may be precancerous or slow-growing.
The pancreatic cancer stages of dying are most commonly associated with advanced PDAC due to its rapid progression.
Causes and Risk Factors
The exact cause of pancreatic cancer is not always known, but several risk factors increase the likelihood of developing the disease:
-
Smoking and tobacco use
-
Chronic pancreatitis
-
Diabetes, especially new-onset diabetes in older adults
-
Family history and genetic mutations (BRCA1, BRCA2, PALB2)
-
Obesity and poor diet
-
Age over 60
These factors can also influence disease progression and survival outcomes.
Symptoms and Early Warning Signs
Early pancreatic cancer often causes subtle symptoms, which contributes to late diagnosis. Common early warning signs include:
-
Unexplained weight loss
-
Loss of appetite
-
Abdominal or back pain
-
Jaundice (yellowing of skin and eyes)
-
Fatigue
As the disease progresses into the pancreatic cancer stages of dying, symptoms may intensify and include:
-
Severe pain requiring strong medication
-
Profound weakness and fatigue
-
Difficulty eating and swallowing
-
Fluid buildup in the abdomen (ascites)
-
Shortness of breath
-
Increased sleep and reduced awareness
Diagnosis
Diagnosis typically involves a combination of:
-
Imaging tests such as CT scans, MRI, or PET scans
-
Endoscopic ultrasound with biopsy
-
Blood tests, including CA 19-9 tumor marker
-
Genetic testing in selected cases
In advanced cases, diagnostic efforts focus more on monitoring symptoms and guiding palliative care decisions rather than extensive testing.
Treatment Options
Treatment depends on the stage at diagnosis:
-
Early stages: Surgery (Whipple procedure), chemotherapy, and radiation
-
Locally advanced stages: Chemotherapy and radiation to slow progression
-
Pancreatic cancer stages of dying: Palliative care, pain management, and symptom control
End-stage treatment prioritizes comfort rather than cure, including pain relief, nutritional support, and emotional care.
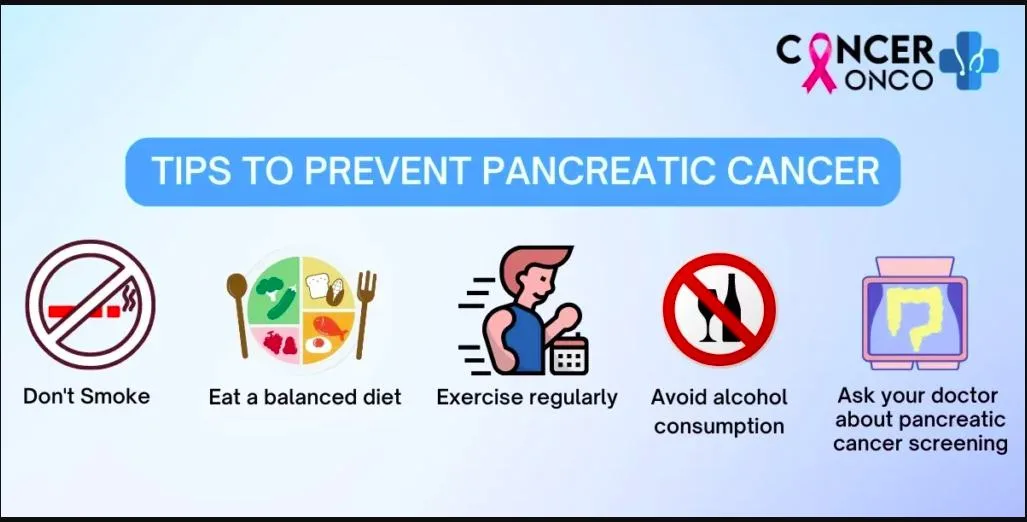
Prevention and Lifestyle Recommendations
While pancreatic cancer cannot always be prevented, certain lifestyle changes may reduce risk and improve overall health:
-
Quit smoking
-
Maintain a healthy weight
-
Eat a balanced diet rich in fruits, vegetables, and whole grains
-
Manage diabetes effectively
-
Seek medical attention for persistent digestive symptoms
For patients in advanced stages, lifestyle recommendations focus on comfort, gentle activity, and emotional well-being rather than prevention.
Prognosis and Survival Rates
Pancreatic cancer has one of the lowest survival rates among cancers. Overall five-year survival is approximately 10–12%. In the pancreatic cancer stages of dying, life expectancy may range from weeks to several months, depending on individual health, response to supportive care, and disease spread.
While these statistics can be difficult to hear, it is important to remember that every patient’s journey is unique.
Latest Research and Innovations
Ongoing research aims to improve early detection and treatment, including:
-
Targeted therapies based on genetic mutations
-
Immunotherapy combinations
-
Liquid biopsies for earlier diagnosis
-
Personalized medicine approaches
Although these advances may not reverse end-stage disease, they offer hope for future patients and ongoing improvements in care.
Coping and Support for Patients
Facing the pancreatic cancer stages of dying is emotionally challenging for patients and families. Support strategies include:
-
Palliative care teams for symptom management
-
Hospice care focusing on dignity and comfort
-
Counseling and mental health support
-
Spiritual care and support groups
-
Open communication with loved ones
Emotional support is just as important as medical care during this time.
Conclusion
Understanding pancreatic cancer stages of dying helps patients and families prepare for what lies ahead with clarity and compassion. While the disease is aggressive and outcomes are often difficult, supportive care, pain management, and emotional support can significantly improve quality of life. Knowledge empowers families to make informed decisions, cherish meaningful moments, and ensure dignity throughout the journey.
FAQ
1. What are the final stages of pancreatic cancer like?
The final stages often involve increased fatigue, pain, reduced appetite, and more time spent sleeping. Palliative care focuses on comfort and symptom relief.
2. How long do patients live in the pancreatic cancer stages of dying?
Life expectancy varies but is often measured in weeks to months, depending on overall health and disease progression.
3. Is pain always severe at the end stage?
Pain can usually be well-managed with modern medications and palliative care techniques.
4. Should hospice care be considered?
Yes, hospice care is highly recommended during the pancreatic cancer stages of dying to support both patients and families.
5. Can quality of life still be maintained?
With proper medical, emotional, and social support, many patients experience comfort, dignity, and meaningful connections even in advanced stages.