Molecular Subtypes of Breast Cancer: Causes and Risk Factors
Breast cancer is a complex disease that affects millions of women worldwide each year. Over the past few decades, research has shown that breast cancer is not a single condition, but rather a collection of different subtypes with unique biological features. Understanding these differences is crucial because they directly influence treatment decisions, prognosis, and long-term survival outcomes.
The concept of molecular subtypes of breast cancer has revolutionized oncology. By classifying breast cancer based on genetic and molecular characteristics, doctors can provide more personalized therapies. This approach helps patients receive treatments that are more effective and less toxic compared to traditional one-size-fits-all strategies.
Definition and Overview
Molecular subtypes of breast cancer are classifications based on the gene expression patterns and receptor status of tumor cells. Instead of only looking at the cancer under a microscope, scientists analyze biomarkers such as estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). These markers, along with genomic profiling, divide breast cancer into clinically significant categories.
This molecular classification system provides essential insights into tumor behavior, aggressiveness, and response to therapies. It has become the foundation for modern breast cancer treatment strategies and clinical guidelines.
Types
There are four main molecular subtypes of breast cancer:
- Luminal A:
- ER-positive and/or PR-positive, HER2-negative.
- Slow-growing with the best prognosis.
- Often responds well to hormonal therapy.
- Luminal B:
- ER-positive and/or PR-positive, may be HER2-positive.
- More aggressive than Luminal A.
- May require a combination of hormone therapy, chemotherapy, and targeted therapy.
- HER2-Enriched:
- HER2-positive, usually ER-negative and PR-negative.
- Fast-growing and aggressive.
- Responds well to HER2-targeted treatments such as trastuzumab.
- Triple-Negative (Basal-like):
- Negative for ER, PR, and HER2.
- Aggressive with fewer targeted treatment options.
- Often treated with chemotherapy and newer immunotherapy approaches.
Causes and Risk Factors
The molecular subtypes of breast cancer are influenced by a combination of genetic, hormonal, and lifestyle factors. Some common causes and risk factors include:
- Family history and inherited genetic mutations (e.g., BRCA1 and BRCA2).
- Hormonal influences, such as prolonged estrogen exposure.
- Lifestyle choices, including poor diet, lack of exercise, and alcohol consumption.
- Environmental exposures and radiation.
- Age, with risk increasing after 40.
Symptoms and Early Warning Signs
Although the molecular subtypes of breast cancer differ biologically, their symptoms often overlap. Common warning signs include:
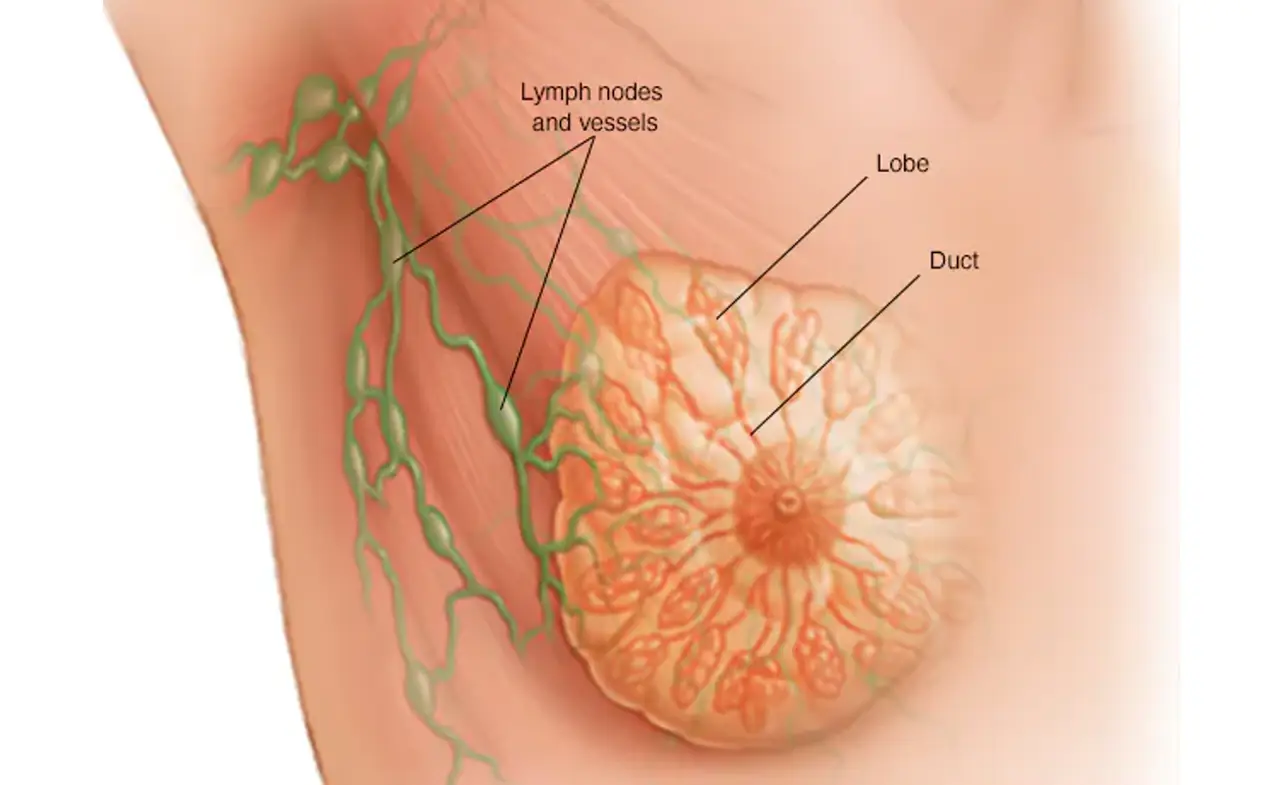
- A lump in the breast or underarm.
- Changes in breast size, shape, or contour.
- Unexplained pain or tenderness.
- Nipple discharge, including blood.
- Skin changes such as dimpling, redness, or thickening.
Early detection plays a key role in improving survival rates across all breast cancer subtypes.
Diagnosis
Diagnosing the molecular subtypes of breast cancer involves several steps:
- Imaging tests: Mammogram, ultrasound, and MRI.
- Biopsy: Removing tissue samples for laboratory analysis.
- Immunohistochemistry (IHC): Testing for ER, PR, and HER2 status.
- Genomic profiling: Advanced testing to determine gene expression patterns.
Accurate diagnosis ensures that patients receive the most suitable treatment plan tailored to their molecular subtype.
Treatment Options
Treatment depends heavily on the molecular subtype of breast cancer:
- Luminal A: Hormone therapy (tamoxifen, aromatase inhibitors).
- Luminal B: Hormone therapy plus chemotherapy or HER2-targeted therapy if HER2-positive.
- HER2-Enriched: HER2-targeted therapy (trastuzumab, pertuzumab) combined with chemotherapy.
- Triple-Negative: Chemotherapy, immunotherapy, and clinical trial options.
Personalized treatment plans improve outcomes and minimize unnecessary side effects.
Prevention and Lifestyle Recommendations
While not all cases can be prevented, certain lifestyle choices can reduce the risk of developing aggressive molecular subtypes of breast cancer:
- Maintain a healthy weight.
- Engage in regular physical activity.
- Limit alcohol consumption and avoid smoking.
- Eat a diet rich in fruits, vegetables, and whole grains.
- Get regular screenings, especially if you have a family history.
Prognosis and Survival Rates
Prognosis varies significantly depending on the subtype:
- Luminal A has the best survival rates due to slower growth and responsiveness to hormone therapy.
- Luminal B has a moderately good prognosis but requires more aggressive treatment.
- HER2-Enriched survival rates have improved dramatically with targeted therapy.
- Triple-Negative has the poorest prognosis due to limited treatment options, though research is rapidly evolving.
Latest Research and Innovations
Recent advancements in breast cancer research are transforming patient care:
- Development of new targeted therapies for HER2-positive cancers.
- Immunotherapy showing promise for triple-negative breast cancer.
- Genomic testing to predict recurrence risk.
- Artificial intelligence in imaging and diagnosis.
These innovations are paving the way toward precision medicine and better survival outcomes.
Coping and Support for Patients
A breast cancer diagnosis can be emotionally overwhelming. Patients should seek support from healthcare professionals, family, friends, and cancer support groups. Psychological counseling, mindfulness practices, and survivorship programs also help improve mental health and quality of life.
Practical support such as financial counseling, patient advocacy, and rehabilitation services play an equally vital role in ensuring holistic recovery.
Conclusion
Understanding the molecular subtypes of breast cancer is essential for advancing treatment and improving survival rates. Each subtype behaves differently and requires a tailored approach to care. With continuous advancements in medical research, patients today have more effective options than ever before.
By combining early detection, personalized treatment, and healthy lifestyle choices, patients can significantly improve their outcomes. Spreading awareness of molecular subtypes empowers individuals to make informed decisions and supports ongoing progress in the fight against breast cancer.
FAQ
1. What are the main molecular subtypes of breast cancer?
The main subtypes are Luminal A, Luminal B, HER2-Enriched, and Triple-Negative.
2. Which breast cancer subtype has the best prognosis?
Luminal A generally has the best prognosis due to its slower growth and responsiveness to hormone therapy.
3. Is triple-negative breast cancer harder to treat?
Yes, triple-negative is more challenging because it lacks targeted receptors, but new therapies are emerging.
4. Can lifestyle changes reduce breast cancer risk?
Yes, maintaining a healthy weight, exercising, and avoiding alcohol and smoking can reduce risk.
5. Are molecular subtypes used in all breast cancer diagnoses?
Yes, modern oncology relies on molecular classification to guide treatment decisions and improve outcomes.