Immunotherapy Drugs for Lung Cancer: Types, Benefits, Survival Rates
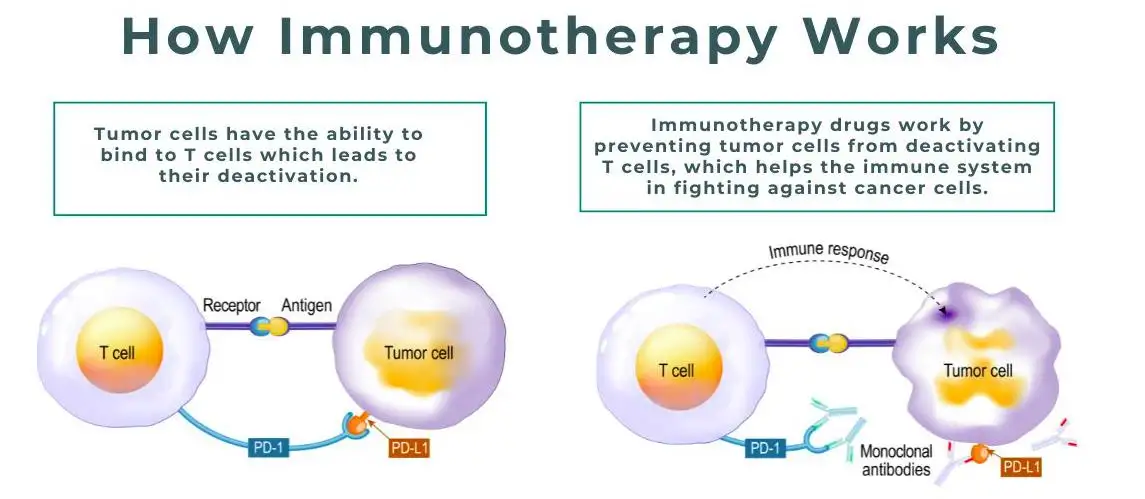
Immunotherapy drugs for lung cancer have transformed the way this serious disease is treated, offering new hope to patients who previously had limited options. Unlike traditional treatments that directly attack cancer cells, immunotherapy works by strengthening the body’s own immune system so it can recognize and fight cancer more effectively. This approach has led to longer survival and improved quality of life for many people with lung cancer.
As research continues to advance, immunotherapy drugs for lung cancer are becoming an essential part of modern oncology care. Understanding how these treatments work, who they are best suited for, and what outcomes patients can expect is crucial for patients, caregivers, and anyone seeking reliable health information.
Overview
Immunotherapy drugs for lung cancer are medications designed to enhance or restore the immune system’s ability to detect and destroy cancer cells. Lung cancer cells often evade immune surveillance by using specific molecular pathways to “hide” from immune attack. Immunotherapy targets these pathways, allowing immune cells to respond more effectively.
These drugs are most commonly used in non-small cell lung cancer (NSCLC), which accounts for the majority of lung cancer cases, but they are also being studied and used in certain cases of small cell lung cancer (SCLC).
Types
There are several main types of immunotherapy drugs for lung cancer, each working through different immune mechanisms.
| Type of Immunotherapy | Examples | How It Works |
|---|---|---|
| Immune Checkpoint Inhibitors | Nivolumab, Pembrolizumab, Atezolizumab | Block proteins that prevent immune cells from attacking cancer |
| PD-1 Inhibitors | Pembrolizumab, Nivolumab | Help T-cells recognize and kill cancer cells |
| PD-L1 Inhibitors | Atezolizumab, Durvalumab | Prevent cancer cells from disabling immune responses |
| CTLA-4 Inhibitors | Ipilimumab | Enhance early immune activation against tumors |
Among these, immune checkpoint inhibitors are the most widely used immunotherapy drugs for lung cancer.
Causes and Risk Factors
While immunotherapy itself does not cause lung cancer, understanding the causes and risk factors of the disease helps determine who may benefit most from these treatments.
Common risk factors include smoking, exposure to secondhand smoke, air pollution, asbestos exposure, genetic mutations, and a family history of lung cancer. Patients whose tumors express certain biomarkers, such as PD-L1, are more likely to respond well to immunotherapy drugs for lung cancer.
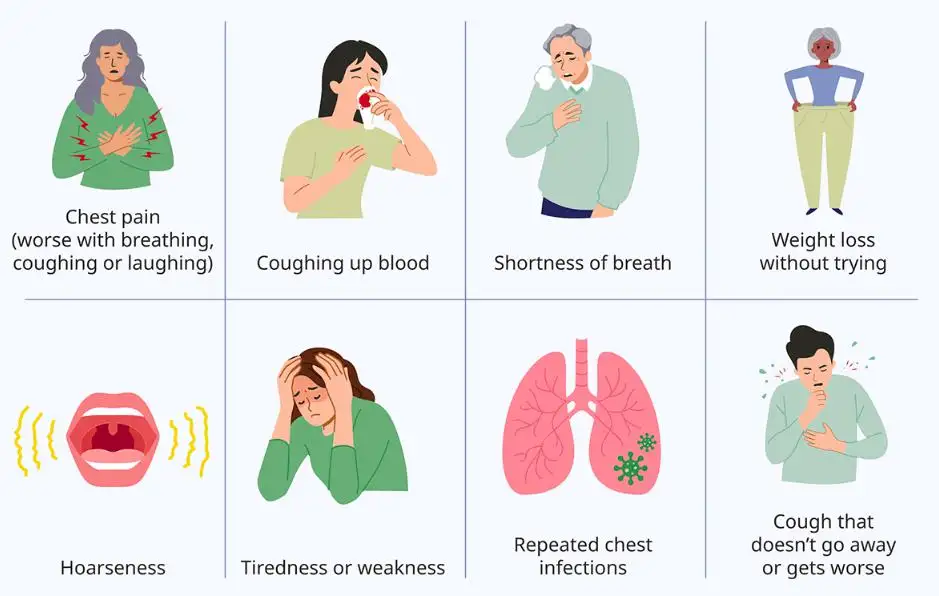
Symptoms and Early Warning Signs
Symptoms of lung cancer can be subtle in early stages, making diagnosis challenging. Early detection improves the effectiveness of treatments, including immunotherapy.
Common symptoms include persistent cough, chest pain, shortness of breath, unexplained weight loss, fatigue, coughing up blood, and recurrent respiratory infections. If these symptoms persist, medical evaluation is strongly recommended.
Diagnosis
Diagnosing lung cancer typically involves imaging studies such as chest X-rays, CT scans, or PET scans, followed by biopsy to confirm cancer type. Molecular and biomarker testing is essential before starting immunotherapy drugs for lung cancer.
Tests for PD-L1 expression, tumor mutational burden (TMB), and specific genetic alterations help doctors determine whether immunotherapy is appropriate and which drug is most likely to be effective.
Treatment Options
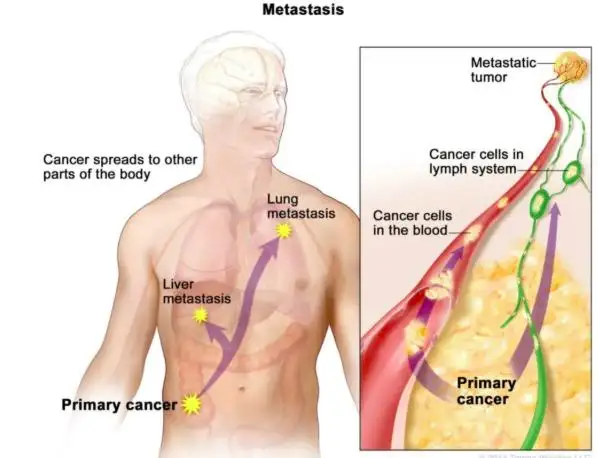
Immunotherapy drugs for lung cancer may be used alone or combined with other treatments, depending on the stage and type of cancer.
| Treatment Approach | When It Is Used |
|---|---|
| Immunotherapy Alone | Advanced or metastatic lung cancer with high PD-L1 expression |
| Immunotherapy + Chemotherapy | First-line treatment for many advanced NSCLC cases |
| Immunotherapy After Chemotherapy | Maintenance or second-line therapy |
| Immunotherapy with Radiation | Selected cases to improve immune response |
Treatment plans are personalized, ensuring patients receive the most effective and safest therapy.
Prevention and Lifestyle Recommendations
While immunotherapy treats lung cancer, prevention remains essential. Avoiding smoking, reducing exposure to environmental toxins, maintaining a healthy diet, exercising regularly, and attending routine health screenings all reduce lung cancer risk.
For patients receiving immunotherapy drugs for lung cancer, lifestyle measures such as balanced nutrition, adequate sleep, stress management, and infection prevention can support immune health and treatment tolerance.
Prognosis and Survival Rates
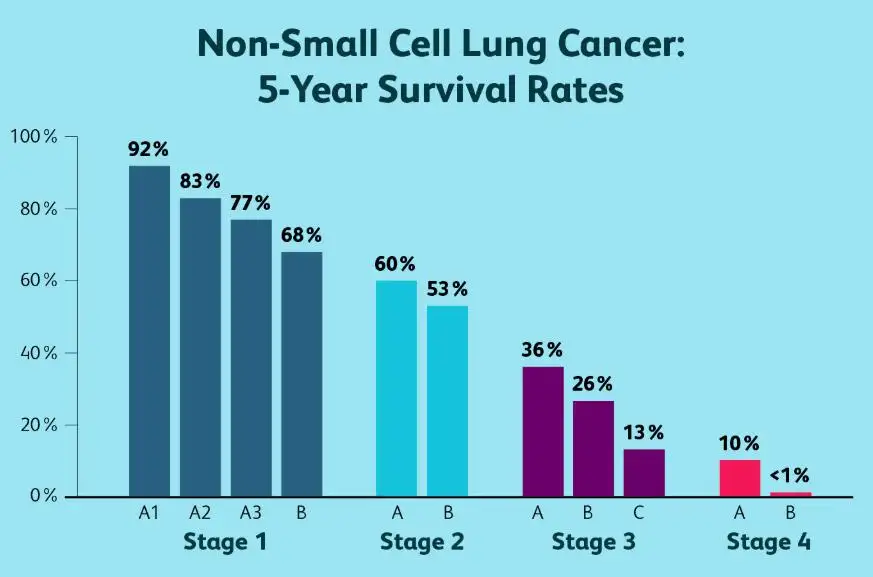
The prognosis for lung cancer has improved significantly with the introduction of immunotherapy. Many patients experience longer survival and better disease control compared to chemotherapy alone.
While survival rates vary based on cancer stage, overall health, and response to treatment, studies show that some patients receiving immunotherapy drugs for lung cancer achieve long-term remission, a result rarely seen in the past.
Latest Research and Innovations
Ongoing research is expanding the role of immunotherapy in lung cancer care. Scientists are developing new checkpoint inhibitors, combination therapies, personalized cancer vaccines, and cell-based treatments.
Clinical trials are also exploring biomarkers to better predict response, reduce side effects, and extend the benefits of immunotherapy drugs for lung cancer to a broader group of patients.
Coping and Support for Patients
Living with lung cancer can be emotionally and physically challenging. Support from healthcare teams, family, friends, and patient advocacy groups plays a vital role in treatment success.
Patients are encouraged to communicate openly with their doctors about side effects, mental health concerns, and quality-of-life issues. Counseling, support groups, and educational resources can help patients feel empowered throughout their immunotherapy journey.
Conclusion
Immunotherapy drugs for lung cancer represent a major breakthrough in cancer treatment, offering improved survival, durable responses, and renewed hope for patients worldwide. As research continues to evolve, these therapies are becoming more effective, personalized, and accessible.
By understanding how immunotherapy works and staying informed about treatment options, patients and caregivers can make confident, informed decisions and actively participate in their care.
FAQ
1. What are immunotherapy drugs for lung cancer?
They are medications that stimulate the immune system to recognize and destroy lung cancer cells.
2. Who is eligible for immunotherapy treatment?
Eligibility depends on cancer type, stage, biomarker test results, and overall health.
3. Are immunotherapy drugs for lung cancer safer than chemotherapy?
They often have fewer traditional side effects, but they can cause immune-related reactions that require monitoring.
4. How long does immunotherapy treatment last?
Treatment duration varies, typically ranging from several months to two years, depending on response and tolerance.
5. Can immunotherapy cure lung cancer?
While not a guaranteed cure, immunotherapy can lead to long-term remission in some patients and significantly extend survival.